Post-Herpetic Neuralgia
Post Herpetic Neuralgia (PHN) is the most common complication of Herpes Zoster-Varicella
(HZV). Pain is sustained for at least 90 days after the rash. It occurs in approximately 20% of
patients with HZV & 80% of cases occur in patients 50 years or older.

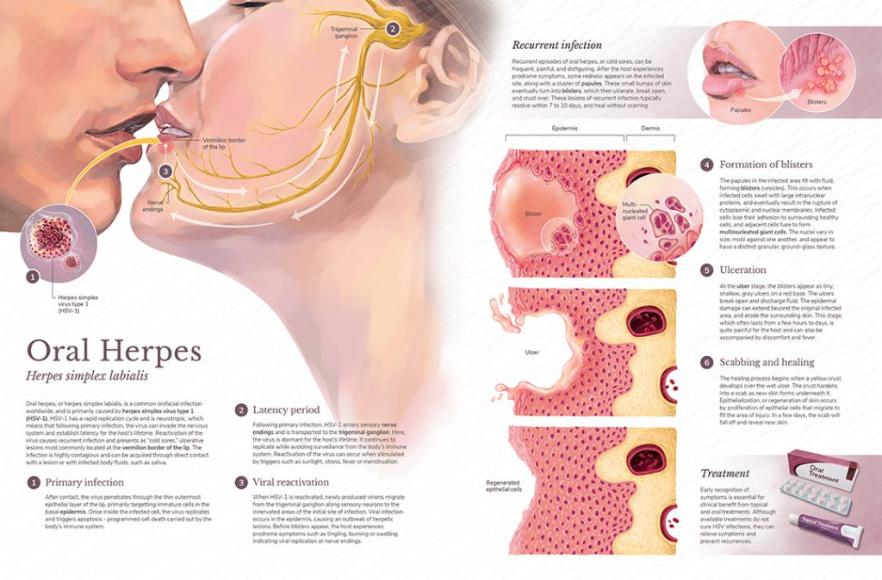
 Photos of Oro-Facial Herpes Zoster-Varicella Infections
Photos of Oro-Facial Herpes Zoster-Varicella Infections

What is Post-Herpetic Neuralgia (PHN)?
PHN is caused by nerve damage secondary to an inflammatory response induced by viral replication within a nerve.
PHN pain is typically discretely localised, intermittent, chronic & sufficiently intense to interfere with sleep & other normal daily activities. Additionally, the pain may have an itching, burning, sharp, stabbing / throbbing quality. PMH may be associated with allodynia / hyperalgesia.
Aggravating factors include light touch, such as the touch of clothing / standing in a shower.
Relieving factors may include barriers to touch.
Risk Factors
These include:
- Older age
- Severe prodrome / rash
- Severe acute HZV pain
- Ophthalmic involvement
- Immunosuppression
- Chronic conditions such as Diabetes Mellitus & Lupus
- Symptoms of allodynia
How is Post-Herpetic Neuralgia treated?
Pain-management strategies should focus on symptom-control.
Although some patients have complete resolution of symptoms after several years, others have to continue using medications indefinitely.
- Capsaicin cream 0.075% cream 3 – 4x daily
- Lidocaine medicated plasters 5% to use for 12 hours & rest for 12 hours
- Antidepressants (Nortryptiline 10 – 125mg / day & Duloxetine 60 – 120mg / day)
- Anticonvulsants (Gabapentin 300 – 600mg mg TDS & Pregabalin 150 – 300mg / day)
- Tramadol 50 – 100 mg 4 – 6 hourly
- Amantidine 100 mg BD for 2/52 – to be continued for another 2/52 if necessary
Referral to specialist clinics (Oral Medicine & Oro-Facial Pain clinics).
 Management of Post-Herpetic Neuralgia
Management of Post-Herpetic Neuralgia
Differential Diagnosis:
The differential diagnosis includes:
- PHN
- Impetigo
- Candidiasis
- Contact dermatitis
- Insect bites
- Auto-Immune blistering diseases
- Dermatitis herpetiformis
- Drug-related eruptions