Mouth-Sinus Holes (Oro-Antral Communications)
What is an Oro-Antral Communication (OAC)?
This is a communication between the maxillary sinus / antrum and the oral cavity / mouth.
What is an Oro-Antral Fistula?
If an OAC is not treated, this can become lined with epithelium (skin). Hence, an oro-antral fistula is an epithelised tract linking the maxillary sinus to the mouth; the tract becomes ‘permanent’.
(Alternative names for an OAC / OAF include oro-antral fistulæ & oral fistulæ, sinus perforations and antra-oral fistulæ).
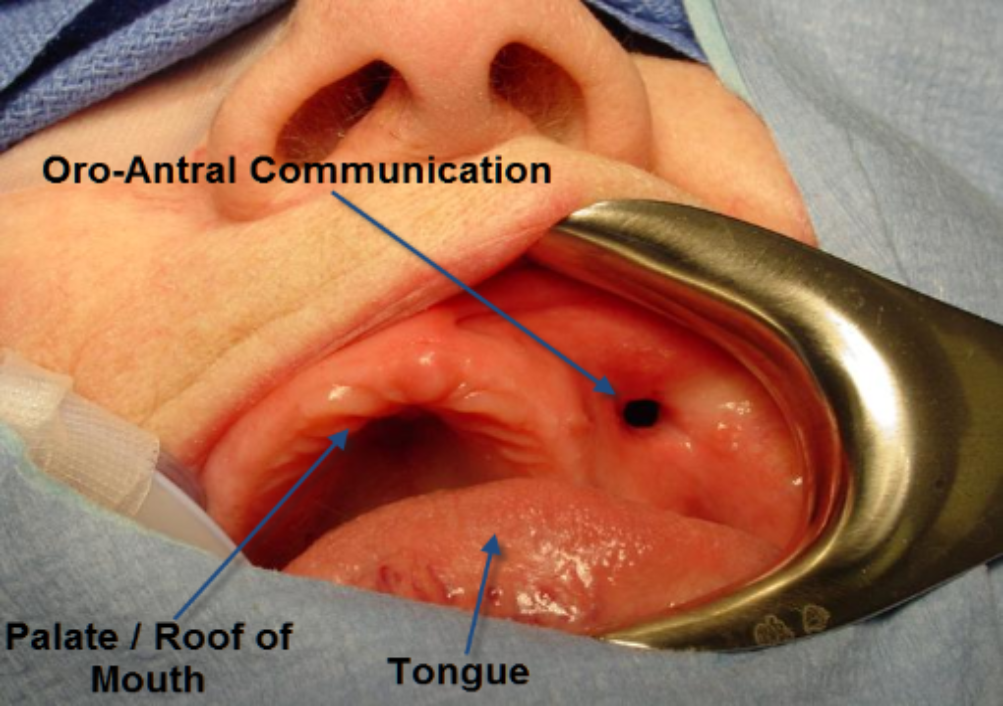

 When an OAC is created, it allows the flow of food, smoke or fluid from the mouth into the nose. Not just these but also bacteria, fungi and viruses. This can set up a maxillary sinusitis, which depending on how long the communication lasts for, may either yield an acute / chronic maxillary sinusitis.
When an OAC is created, it allows the flow of food, smoke or fluid from the mouth into the nose. Not just these but also bacteria, fungi and viruses. This can set up a maxillary sinusitis, which depending on how long the communication lasts for, may either yield an acute / chronic maxillary sinusitis.
Causes of OAC’s:
The vast majority of OAC’s are created when upper molars and premolars are removed (almost 50%), tumours (18.5%), bone infections (osteomyelitis) (11%), operations to access the maxillary sinus (Caldwell-Luc procedures) (7.5%), trauma (7.5%), dentigerous cysts (3.7%), correction of septal perforations (3.7%), perforation of the sinus floor from the tooth socket when trying to remove an upper tooth and localised florid gum disease (HIV-related periodontitis) or tooth-tip infections (chronic apical infection).
Predictive Factors:
As a very broad generalisation, the following may be thought to predispose to an OAC being formed:
- Proximity of sinus floor / tuberosity
- Thickened tooth cement (hypercementosis) / tooth fused to jaw bone (ankylosis)
- Infected teeth / long-standing decay
- Marked periodontitis / gum disease
- Lone-standing
- Previous history of OAC’s.
Treatment of the Acute OAC:
If an OAC has been created, then:
- Do not probe the defect
- Promote good blood clot
- The gingival / gum margins around the socket should be approximated as close as possible
- Physical agents placed in the socket to stop excess bleeding (Surgicel, Spongostan or Haemocollagene)
- Antibiotics should be prescribed (Amoxycillin, Doxycycline)
- Nasal decongestants can be used (Ephedrine nasal drops, Oxymetazoline)
- Steam inhalations can be used (Menthol & Eucalyptus)
- Antiseptic mouth-wash should be used (Corsodyl)
- No nose-blowing or smoking
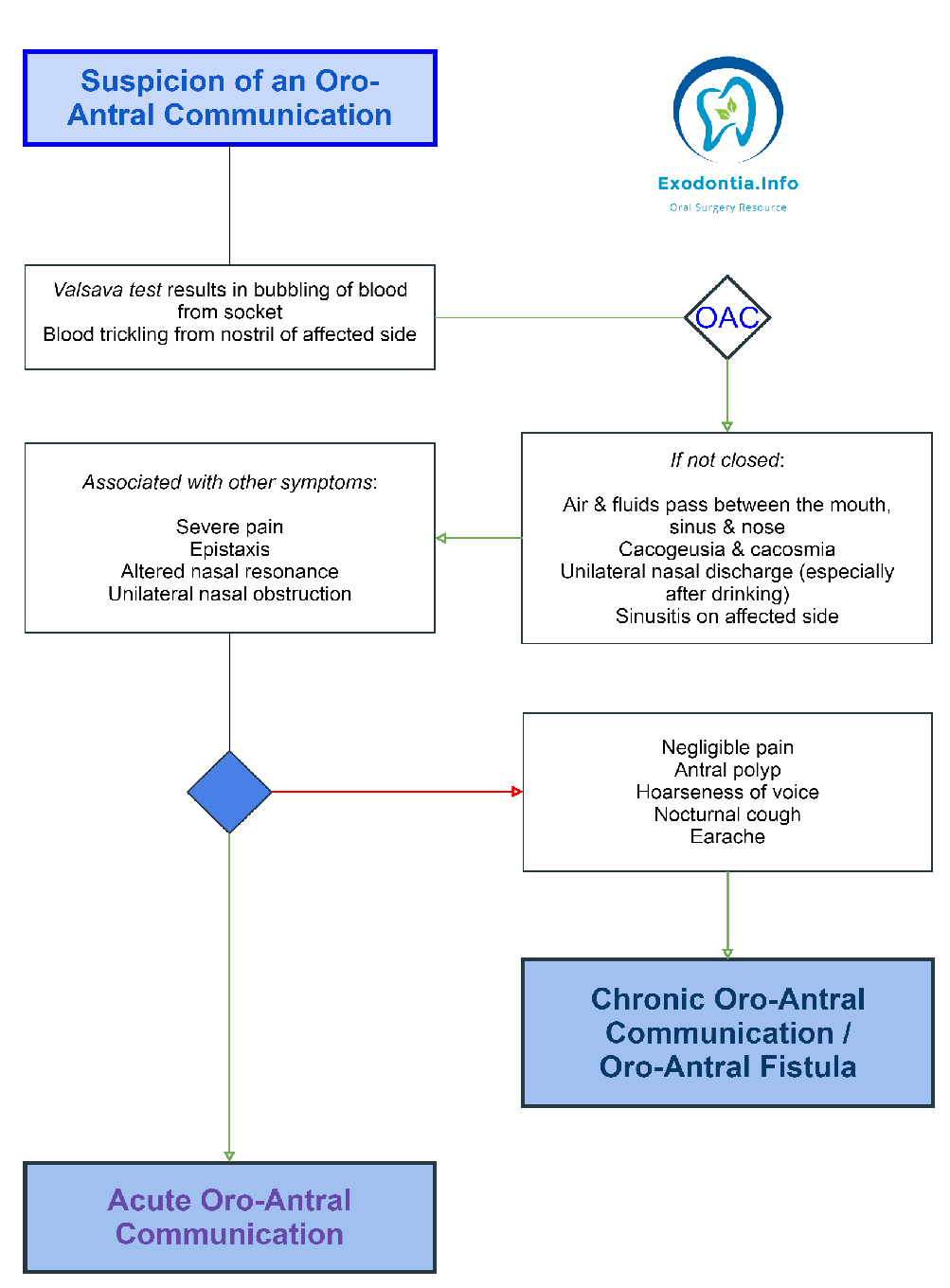
How to Recognise the Chronic OAC / OAF:
The OAC is likely to become chronic if:
- OAC is greater than 5mm in diameter
- Gingival tissues / gums around the socket can’t be approximated
- Post-op régime is not followed
- Wound dehiscence / breakdown
- Enucleation of a dental / dentigerous cyst
- May develop 4 – 6 weeks post-extraction
- Problems with smoking, eating or drinking
- Cacogeusia / foul taste
- Chronic maxillary sinusitis
- Antral polyp herniating into the mouth
- Purulent (pus) discharge from nose
Treatment of the Chronic / Larger OAC / OAF:
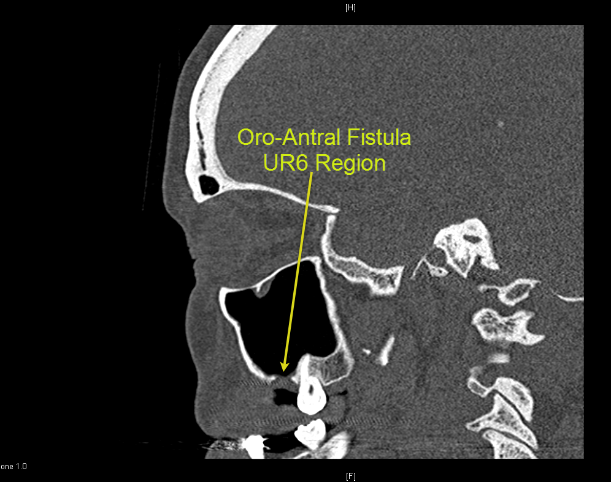
- The OAC is assessed with X-rays & CT’s.
- The OAC may still spontaneously close if a cover plate used.
- If the OAC / OAF needs closing, pre-op antibiotic & decongestant régime (starting 3 – 7 days pre-op).
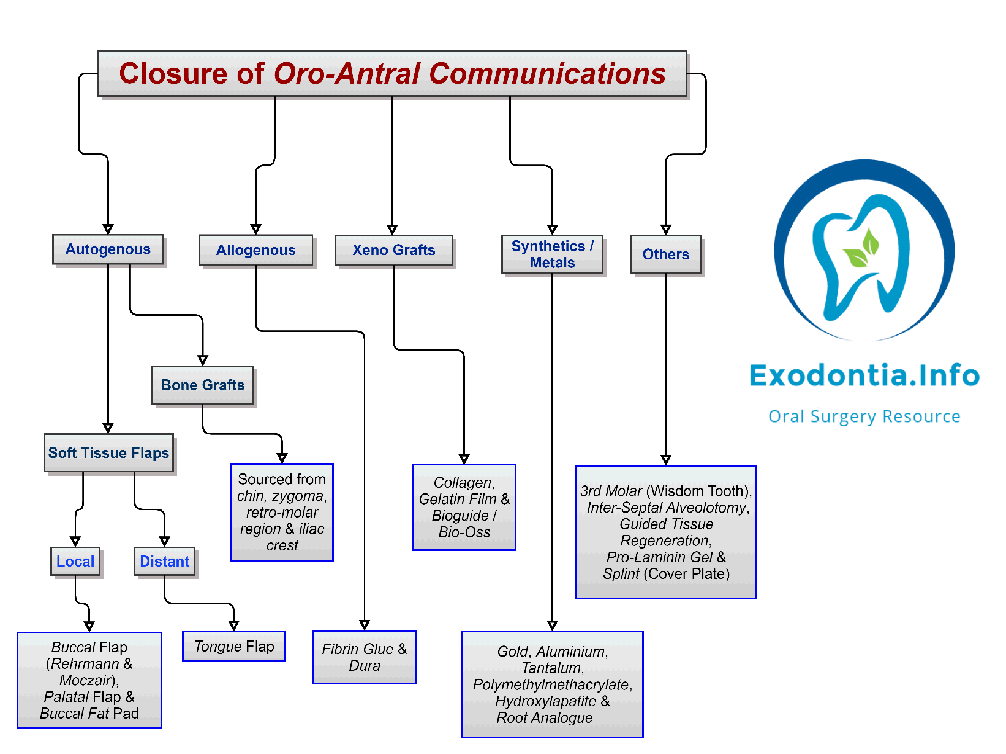
The OAF is closed using the following flaps:
Buccal Flaps:
Buccal Advancement Flap most common. Described by Rehrmann & made popular by Berger.
Palatal Flaps:
- Palatal Rotational Advancement Flap most common.
- Others include Palatal Pedicle Island Flap (Henderson),
- V-shaped Palatal Flap (Krueger) &
- Split-Thickness Palatal Flap (Ito & Hara).
Post-op Régime:
- Antibiotics (Amoxycillin, Doxycycline)
- Analgesics
- Nasal decongestants (Ephedrine nasal drops, Oxymetazoline)
- Steam inhalations (Menthol & Eucalyptus)
- Antiseptic mouth-wash (Corsodyl)
- No nose-blowing or smoking
Useful Articles & Websites
BJOMS 1986. Oro-Antral Fistulae – A Study of Clinical, Radiological & Treatment Aspects
Acta Stomat Croat 2002. Treatment of Oro-Antral Fistula
Swiss Med Wkly 2003. The reconstruction of oral defects with buccal fat pad
Turk J Med Sci 2004. Buccal Corticotomy for Closure of Oro-Antral Openings – Case Report
JOMS 2009. Closure of Oroantral Communications with Bichat’s Buccal Fat Pad
JSCR 2010. Oro-Antral Fistula from Bisphosphonates-Induced Osteonecrosis of the Jaw
JOMS 2010. Closure of Oroantral Communications – A Review of the Literature
Med Oral Patol Oral Cir Bucal. 2010. Oroantral Communications. A Retrospective Analysis
Pakistan Oral & Dent J 2010. Treatment of Oroantral Fistula & A Study
BDJ 2011. Oro-Antral Fistulae & Fractured Tuberosities
Eur Soc Radiology 2011. Oroantral Fistulas. CT Evaluation with Dentascan software
Int J Dent Clinics 2011. Use of Palatal Rotation Flap in the Closure of Oroantral Communication
JUMDC 2012. Case Report. Use of Buccal Fat Pad Oro-Antral Fistula Repair
Open Dent J 2012. Surgical Options In Oroantral Fistula Treatment
JOMS 2013. Treatment of Oro-Antral Fistulas using Bony Press-Fit Technique
J Clin Exp Dent 2015. Alternative Surgical Management of Oroantral Fistula using Auricular Cartilage
Annals of Otolaryngology & Rhinology 2016. Etiology & Management of Oro-Antral Fistula.
J Craniofac Surg 2016. Surgical Treatment of Oro-Antral Communications
Intech 2016. Management of the Oroantral Fistula
World J Plast Surg 2017. Management of Oro-antral Communication & Fistula – Various Surgical Options
Int J Adv Res 2018. Treatment Techniques for Oro-Antral Communications & Fistulas