Cranial Arteritis (Temporal / Giant Cell Arteritis)
What is Cranial Arteritis / Giant Cell Arteritis / Temporal Arteritis / Horton’s Disease?
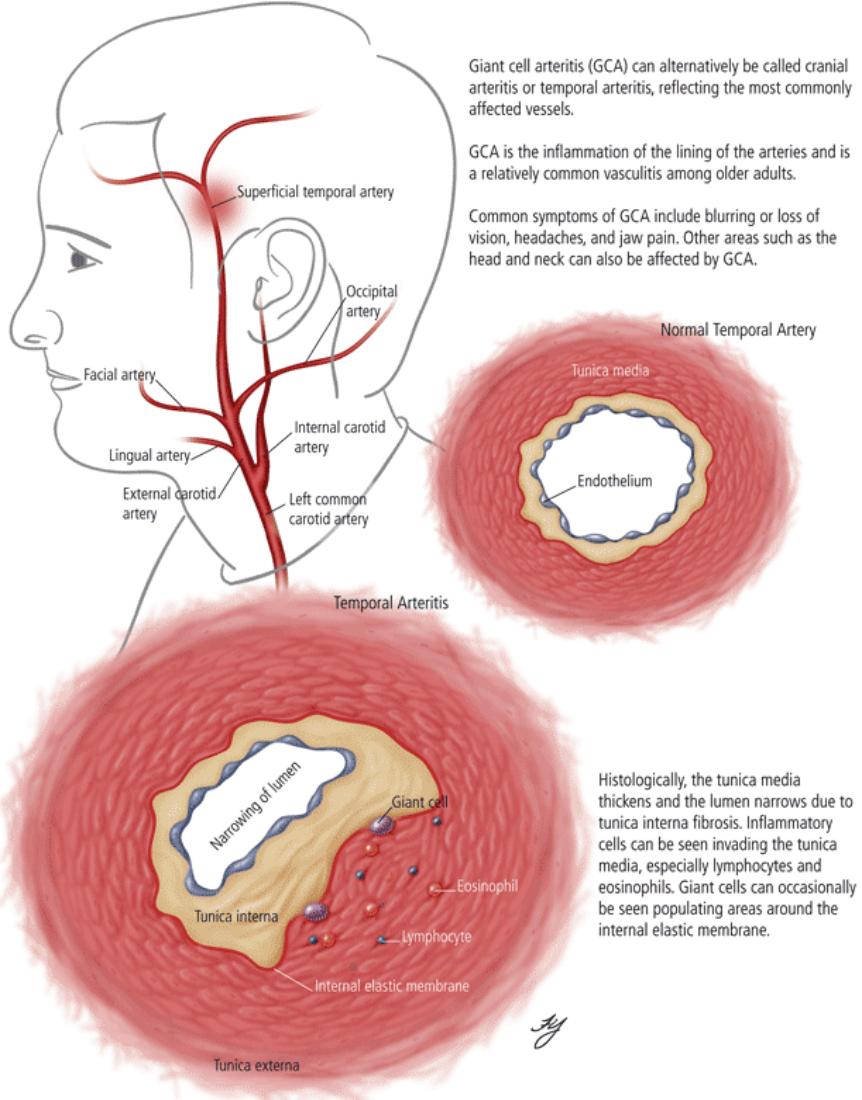
Giant Cell Arteritis (GCA) is an inflammatory disease of the head). It is a form of vasculitis. The inflammation causes the arteries to become narrow, restricting blood flow in the head. It is a serious disease that varies in severity but can often be treated successfully.
The exact cause of GCA is unknown, but it is thought to be an auto-immune reaction (one in which the immune system reacts inappropriately) in the lining of the arteries.
The name, Giant Cell Arteritis, reflects the type of inflammatory cell that is involved (as seen on biopsy).
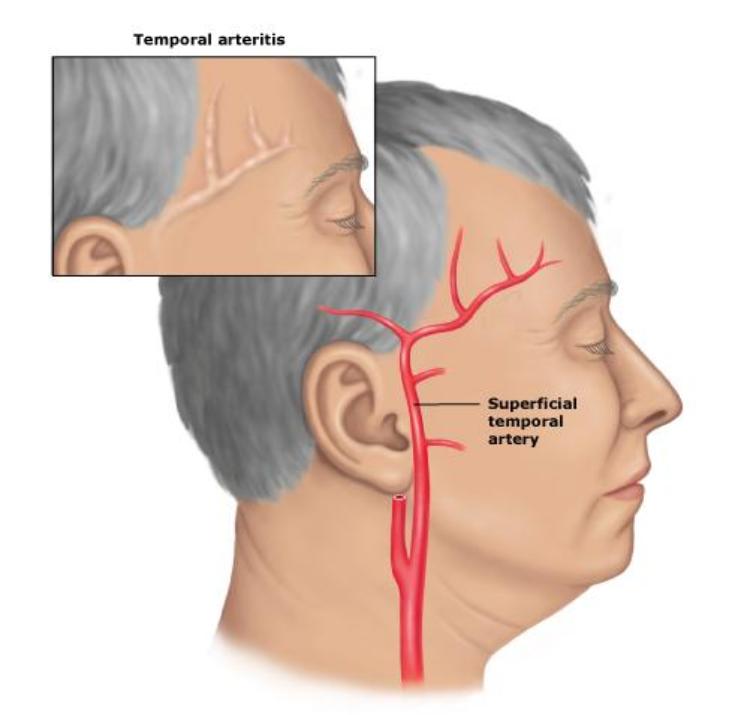
The name, Temporal Arteritis, indicates that the Temporal Artery, which runs over the temple near the ear, is affected. Other arteries such as the Aorta, may be affected, especially those that supply the head and eyes.
What are the signs & symptoms?
Physical Exam
- Palpation of the head reveals prominent temporal arteries with or without pulsation.
- The temporal area may be tender.
- Decreased pulses may be found throughout the body.
- Evidence of ischemia may be noted on fundal exam.
Laboratory Tests
- Erythrocyte Sedimentation Rate (ESR), an inflammatory marker, > 60 mm / hour (normal 10 – 40 mm / hour), but may be normal in approximately 20% of cases.
- C-reactive protein, another inflammatory marker, isalso commonly elevated.
- Platelets may also be elevated.
Investigations
Biopsy. The gold standard for diagnosing GCA is biopsy, which involves removing a small part of the vessel and examining it microscopically for giant cells infiltrating the tissue. Since the blood vessels are involved in a patchy pattern, there may be unaffected areas on the vessel and the biopsy might have been taken from these parts.
Unilateral biopsy of a 1.5 – 3 cm length is 85 – 90% sensitive. So, a negative result does not definitely rule out the diagnosis.
Imaging studies. Radiological examination of the temporal artery with ultrasound yields a halo sign. Contrast enhanced brain MRI and CT is generally negative in this disorder. Recent studies have shown that 3T MRI using super high resolution imaging and contrast injection can non-invasively diagnose this disorder with high specificity and sensitivity.
GCA – Key Features
- Women, usually over 55 years, predominantly affected
- Weakness, low-grade fever and weight-loss often early features
- Severe throbbing headache is a major symptom
- The Temporal Artery frequently becomes red, tender, firm, swollen and tortuous
- Ischæmic pain in the masticatory muscles prominent in 20%. Pain on mastication (chewing), comparable to and often misnamed, jaw claudication (claudication is literally, limping), is sometimes the main symptom and present in about 20% of patients.
- ESR usually greatly raised
- Disturbances of vision or sudden blindness due to involvement of the ophthalmic artery develops in 50% of untreated patients.
- Good response to early treatment with corticosteroids
- Polymyalgia rheumatica, with weakness and pain of the shoulder or pelvic girdles and fever may be associated.
What are the causes of Cranial Arteritis / Giant Cell Arteritis?
Inflammation involves the arterial media and intima (layers within the blood vessel wall). Infiltration by mononuclear cells is typically associated with giant cells (immune and inflammatory cells). Intimal damage leads to formation of thrombi (blood clots), which usually become organised and there may be severe damage to the internal elastic lamina, sometimes going on to complete destruction. Healing is by fibrosis (scarring), particularly of the media, thickening of the intima, and partial re-canalisation of the thrombus (blood clot).
The risk of blindness makes it essential to start treatment early. Systemic corticosteroids (starting with 60 mg/day) a high (> 60 mm / h) ESR. Corticosteroids are usually quickly effective and should be continued until the ESR falls to normal
Lesions skip short lengths of an artery and a biopsy should be at least 3 cm long.
Corticosteroids, typically high-dose prednisone (40 – 60 mg BD), must be started as soon as the diagnosis is suspected (even before the diagnosis is confirmed by biopsy) to prevent irreversible blindness secondary to ophthalmic artery occlusion (blockage).
Steroids do not prevent the diagnosis from later being confirmed by biopsy, although certain changes in the histology may be observed towards the end of the first week of treatment and are more difficult to identify after a couple of months.
The dose of steroid, such as prednisone is lowered after 2 – 4 weeks and slowly tapered over the course of 9 – 12 months. Oral steroids are at least as effective as intravenous steroids, except in the treatment of acute visual loss where intravenous steroids appear to offer significant benefit over oral steroids.
Useful Articles & Websites
Emedicine (Emergency Medicine)
Emedicine (Temporal Artery Biopsy, Clinical Procedure)
NHS Clinical Knowledge Summaries
Ottawa Head Ache Clinic. Temporal Arteritis.
J American Medical Association 2002. Temporal Arteritis.
MJA 2002. Lessons from Practice – Lingual Arteritis In An Elderly Woman.
Orphanet Encyclopædia 2003. Giant Cell Arteritis.
J Chin Med Assoc 2005. Temporal Arteritis.
OT 2005. Giant Cell Arteritis – Emphasis on the Temporal Artery Biopsy.
EULAR Recommendations for the Management of Large Vessel Vasculitis 2008.
BSR and BHPR Guidelines for the Management of Giant Cell Arteritis 2010
Map of Medicine 2010. Temporal Arteritis – Giant Cell Arteritis (Suspected)
BDJ 2012. Letter to Editor. Undiagnosed Temporal Arteritis
BJOMS 2012. Short communication. Giant cell Arteritis — An Incidental Finding