Eagle Syndrome
(Stylohyoid Syndrome / Styloid Syndrome / Styloid-Stylohyoid Syndrome & Styloid–Carotid Artery Syndrome)
What is Eagle Syndrome?
Eagle syndrome (ES) represents symptoms brought on by compression of regional structures by elongation of the styloid process or ossification (calcification) of the stylo-hyoid / stylo-mandibular ligaments.
Patients with ES may present with a sore throat, ear pain, or even with foreign body symptoms in the pharynx secondary to pharyngeal & cervical nerve interactions.
Since the symptoms are variable and non-specific, patients seek treatment in several different clinics such as Ear, Nose & Throat, GP’s, Neurology, Neurosurgery, Psychiatry, and the last but not the least Dentistry / Oral & Maxillofacial Surgery.
It was described in 1937 by Watt Eagle.
What are the Signs & Symptoms of Eagle Syndrome?
Depending on the underlying pathogenetic mechanism and the anatomical structures compressed or irritated by the styloid process, symptoms vary greatly, ranging from cervico-facial pain to cerebral ischæmia.
Clinical presentation is varied and establishing a causative relationship between the styloid process / stylohyoid ligament and symptoms can be challenging.
The syndrome can be divided into 2 main subtypes:
due to compression of cranial nerves (Trigeminal, Facial, Glossopharyngeal, & Vagus nerves) & due to compression of carotid artery
 Anatomical Structures in the Neck involved in Eagle Syndrome
Anatomical Structures in the Neck involved in Eagle Syndrome
What are the Signs & Symptoms of Eagle Syndrome?
Depending on the underlying pathogenetic mechanism and the anatomical structures compressed or irritated by the styloid process, symptoms vary greatly, ranging from cervico-facial pain to cerebral ischæmia.
Clinical presentation is varied and establishing a causative relationship between the styloid process / stylohyoid ligament and symptoms can be challenging.
The syndrome can be divided into 2 main subtypes:
due to compression of cranial nerves (Trigeminal, Facial, Glossopharyngeal, & Vagus nerves) & due to compression of carotid artery
Cranial Nerve Impingement
Patients can have symptoms related to compression and irritation of cranial nerves in the region (cranial nerves V, VII, IX and X) such as:
- facial pain while turning the head
- facial paræsthesia (numbness)
- dysphagia (problems swallowing)
- foreign body sensation (globus hystericus)
- pain on extending tongue
- change in voice (lasting for only a few minutes)
- sensation of hypersalivation
- tinnitus or otalgia
On palpation of the styloid process tip, symptoms should ideally be exacerbated.
(Carotid) Arterial Impingement
Compression of the Carotid Artery may also produce vascular / ischæmic symptoms as well as pain along the artery to the supplied territory (thought to be mediated by the [ortho-]sympathetic plexus) including:
- mechanical compression such as visual symptoms, syncope (fainting) & carotid dissection
- (ortho-) sympathetic plexus irritation (carotidynia) such as eye pain & parietal pain
What are the Causes of Eagle Syndrome?
In most cases, the cause is not known however the condition is sometimes associated with disorders causing heterotopic calcification / ossification such as abnormal Calcium-Phosphorus metabolism and chronic renal failure.
The cause of onset of pain in patients previously free of symptoms is unknown, but several mechanisms have been proposed that include:
- rheumatic styloiditis caused by pharyngeal infections
- trauma
- tonsillectomy, and
- involutional changes associated with ageing (e.g., degenerative cervical discopathy, which may shorten the cervical spine and alter the direction of the styloid process).
The patho-physiological mechanisms for the pain of ES include:
- Compression of the neural elements, the glossopharyngeal nerve, lower branch of the trigeminal nerve, and / or the chorda tympani by the elongated styloid process
- Fracture of the ossified stylohyoid ligament, followed by proliferation of granulation tissue that causes pressure on surrounding structures & results in pain
- Impingement on the carotid vessels by the styloid process, producing irritation of the sympathetic nerves in the carotid arterial sheath
- Degenerative & inflammatory changes in the tendonous portion of the stylohyoid insertion (insertion tendinosis)
- Irritation of the pharyngeal mucosa by direct compression by the styloid process
- Stretching & fibrosis involving the V, VII, IX & X cranial nerves
The mere presence of an elongated styloid process or mineralisation of the stylohyoid complex radiographically in the presence of cervico-pharyngeal pain does not automatically confirm a diagnosis of ES.
There are reasons from 3 aspects.
1. Many patients with an ossified stylohyoid complex are asymptomatic.
2. There does not appear to be any correlation between the severity of pain & the extent of ossification of the stylohyoid complex.
3. The majority of symptomatic patients have had no recent history of surgery (such as a tonsillectomy) or any other cervico-pharyngeal trauma.
Who does it affect?
ES is a rare disease. 0.04 – 0.08% of population suffers from ES, whereas 1.5 – 3.0 % of adults have some of the complaints due to the pathology of the styloid apparatus.
ES occurs mainly in 30 – 50-year-old patients as regional ligaments & the soft tissues of the styloid process become less elastic with age & offer more resistance to surrounding hard tissue structures. However, it has also been reported in children.
Do I need any special tests?
The diagnosis of ES must be based on a good medical history & physical examination.
It should be possible to feel an elongated styloid process by careful intra-oral palpation, placing the index finger in the tonsillar fossa and applying gentle pressure.
If pain is reproduced by palpation & either referred to the ear, face or head, the diagnosis of an elongated styloid process is very likely. A styloid process of normal length is usually not palpable. Injection of local anaesthetic into tonsillar fossa relives pain and can be used as a diagnostic tool.
The diagnosis of ES can be ascertained with imaging which includes lateral head and neck radiographs, Towne radiograph, OPG, lateral-oblique mandible plain film etc.
Radiographic Features
The normal length of the adult styloid in an adult thought to be approximately 2.5 cm while an elongated styloid is considered > 3 cm. If this definition is used, ~4% of the population have an elongated process, however only a small proportion of them (4 – 10%) are symptomatic. Elongation can be unilateral or bilateral.
When mechanical vascular compression is potentially the cause of ischæmic symptoms that angiographic examination (CT angiography / catheter angiography) obtained with the patient’s head positioned to reproduce symptoms may demonstrate mechanical stenosis of the carotid artery.
Imaging only demonstrates elongation of the styloid process and proximity to surrounding key structures. The diagnosis of ES is based on multiple clinical and radiographic factors.
 OPG showing bilateral calcified styloid processes
OPG showing bilateral calcified styloid processes
 CT showing bilateral calcified styloid processes
CT showing bilateral calcified styloid processes
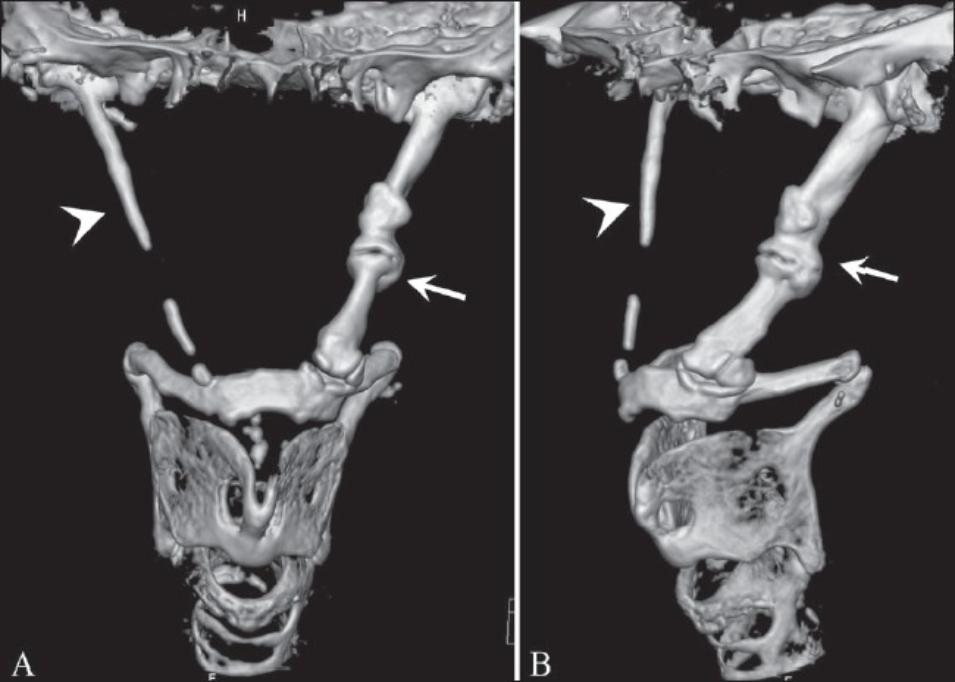
 3D CT showing bilateral calcified styloid processes
3D CT showing bilateral calcified styloid processes
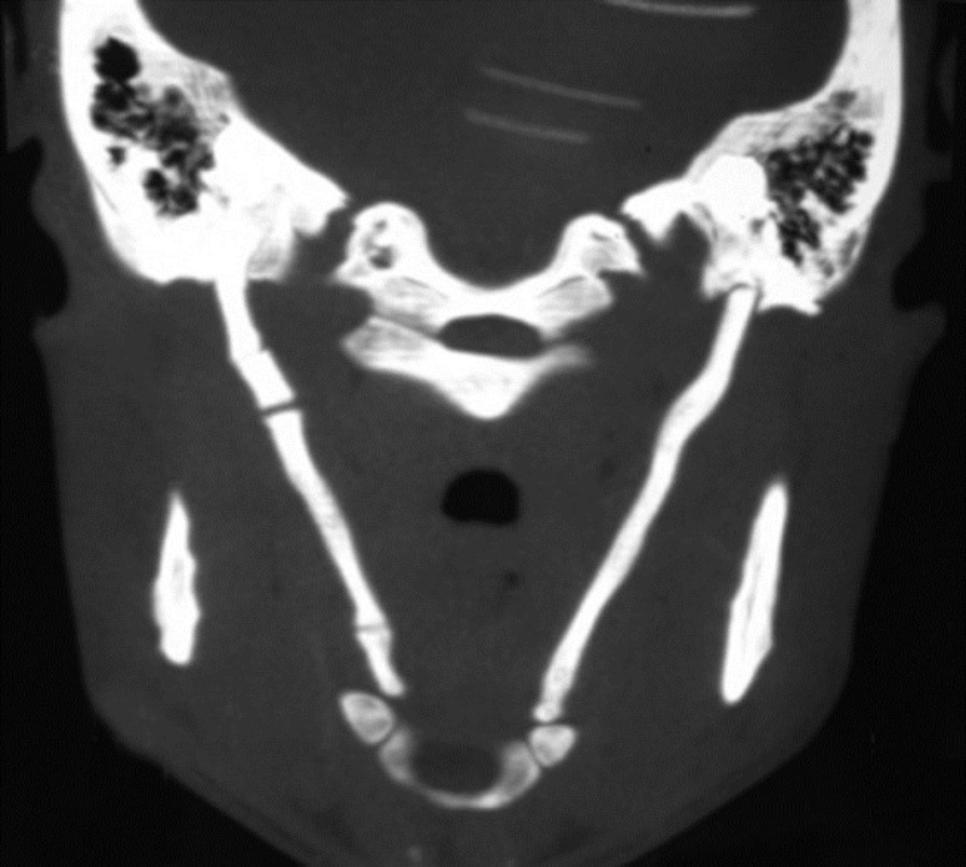 CT showing bilateral calcified styloid processes & ligaments (below)
CT showing bilateral calcified styloid processes & ligaments (below)
How is it treated?
In many cases, once the cause of pain has been attributed to the styloid process rather than a more sinister entity, no further treatment is required, perhaps supplemented with analgesics.
- Trans-pharyngeal injection of steroids / local anæsthetics. Use of LA can be used as a confirmatory procedure.
- Anti-epileptic preparations. Carbamazepine (600mg – 800mg / day) for 2 – 3 weeks
- Anti-histamines
- Application of heat
- Traditional Chinese medicines
- Trans-pharyngeal manipulation with manual fracturing of the styloid process
- The supporting component consists of the medicaments widening the blood vessels, neuroleptics, antidepressants & tranquilizers.
The most satisfactory & effective treatment is surgical shortening of the styloid process through either an intra-oral or extra-oral approach.
The most significant advantage of an external approach is enhanced exposure of the styloid process & the adjacent structures & this outweighs all other considerations. It also facilitates the resection of a partially ossified stylohyoid ligament. Trans-oral resection causes no outside scars, but involves the risk of deep cervical infection & possible neuro-vascular injury. Persistent pain even after surgical excision may be as high as 20%.
Prognosis of ES is guarded by surgical failures (up to 20% of patients). This may be due to intra-operative injury, subsequent fibrous entrapment syndrome or inadequate shortening of the styloid process, assuming that the diagnosis was correct in the first place.
Differential Diagnosis
A differential diagnosis of ES should include:
- laryngo-pharyngeal dysæsthesia
- trigeminal / glossopharyngeal neuralgia, neuralgia of sphenopalatine ganglia
- TMJ disorders, temporomandibular arthritis, cervical vertebral arthritis, temporal arteritis
- temporal rachitis
- chronic tonsillo-pharyngitis
- hyoid bursitis, Sluder’s syndrome, histamine cephalgia
- esophageal diverticula
- benign or malign neoplasms
- cluster type headache, migraine type headache
- dental malocclusion, unerupted or impacted molar teeth & faulty dental prostheses
Useful Articles & Websites
Austral Dent J 1997. Eagle’s Syndrome Masquerading as Pain of Dental Origin. Case Report
BDJ 1999. Eagle’s Syndrome – An Unusual Cause of a Clicking Jaw
JCCA 2003. Eagle’s Syndrome – A Case of Symptomatic Calcification of the Stylohyoid Ligaments
Diagn Interv Radiol 2005. Three-Dimensional CT of Eagle’s Syndrome
JOMS 2007. Styloid-Stylohyoid Syndrome (Eagle’s Syndrome). Literature Review & Case Report
Eur Rev Med & Pharmacol Sci 2008. Atypical Chronic Head & Neck Pain – Don’t Forget Eagle’s Syndrome
OHDMBSC 2010. Case Report of a 27-Year-Old Patient Suffering From Eagle’s Syndrome
Saudi Dent J 2011. Case Report. Eagle’s Syndrome – A Case Report & Review of the Literature
Int Arch Otorhinolaryngol 2013. Case Report. Eagle’s Syndrome