Minor Salivary Gland Biopsy
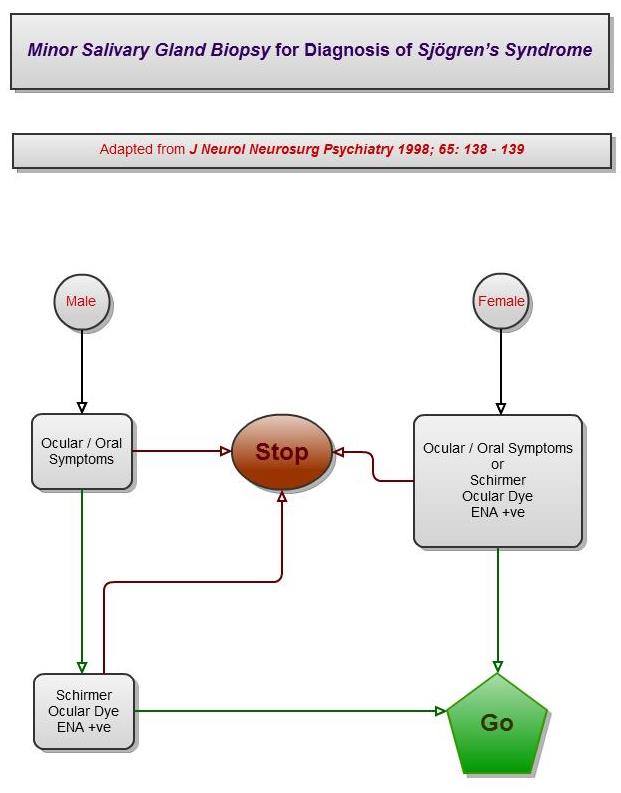
In suspected cases of Sjögren’s Syndrome, patients are often referred for a lower lip minor salivary gland biopsy.
The minor salivary gland biopsy by itself will not diagnose time the biopsy happens, the patient would have already had a number of other clinical, blood, functional and morphological investigations [as laid out by the American-European Consensus Group]).
Biopsy of the minor salivary glands of the lower lip has been used for many years as the changes in the lower lip mirror those in the major salivary glands (parotid and submandibular glands). The presence of chronic inflammatory cells in lip salivary glands, as assessed with the minor salivary gland biopsy, is one of the parameters included in most criteria sets proposed for Sjögren’s Syndrome classification.
What is a Minor Salivary Gland Biopsy & How Is It Done?
A Minor Salivary Gland biopsy is a procedure where an incision is made within the lower lip and minor salivary glands present just below the surface are plucked out and looked at closely under a microscope. It is a relatively minor and safe procedure.
A local anæsthetic injection is used to numb the area which takes a couple of minutes to work. After this injection, the procedure should be painless. An incision, needing stitching afterwards, is made to the lower lip. The stitches dissolve after 10 – 14 days. All together, this procedure usually takes around 15 – 20 minutes from start to finish.
Is there much soreness afterwards?
When the anæsthetic wears off, there will be some pain and discomfort. Simple painkillers will usually be effective. You will be advised which are the best to take. Any discomfort usually only lasts a few days.
Will there be much bleeding?
Although there may be a little bleeding at the time of the biopsy, this usually stops very quickly and is unlikely to be a problem if the wound is stitched. When you get home, should the biopsy site bleed again, apply pressure over the area for at least 10 minutes with a rolled up handkerchief or swab (if you have been given one). This should stop the bleeding but if the bleeding continues please contact your Oral Surgeon / OMFS Department.
When can I return to work?
This largely depends on your job and how you feel after the procedure. Most people are able to return to work later the same day.
Will I need another appointment?
A follow-up appointment is not always necessary but you will usually be asked to attend an appointment for the results of the biopsy to be discussed with you. A care advice leaflet will be given to you after the biopsy.
Minor Salivary Gland Biopsy – Operation Warnings
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004] [https://exodontia.info/chester-vs-afshar-2004/], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
The following list of warnings regarding minor salivary gland biopsies is neither exhaustive nor is it predictive.
The most pertinent warnings have been included here.
As it is a surgical procedure, there will be soreness after the procedure. This can last for several days. Painkillers such as ibuprofen or paracetamol are very effective. Obviously, the analgesic you use is dependent on your medical history and the ease with which the biopsy was carried out.
Swelling.
There will be swelling afterwards. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that will develop.
Stitches.
The biopsy site will be closed with stitches. These are dissolvable and & will “fall out” within 10 – 14 days.
Scarring / Lumpiness at Biopsy Site.
Any cut to soft tissues produces a scar. Initially, after a biopsy, a scar will be produced. This softens and disappears (i.e. improves) with time. Regardless, it can feel quite obvious and lumpy to begin with. The scarring can also dependent on the size and size of the biopsy and the individual’s tendency to scarring.
Initial Tautness / Tenderness at Biopsy Site.
To close the biopsy site, the wound margins are closed with stitches. These place tension and hence tenderness at the biopsy site; this tails off with time.
Localised Area of Numbness at Biopsy Site.
The biopsy can damage the local nerves resulting in areas of numbness. These can take a number of months before normal feeling returns.
Inconclusive Results & the Need for Re-biopsy.
The biopsy results can come back as inconclusive. If this is the case, then it is possible that the biopsy will need to be repeated.
Further treatment dependent on Results.
Depending on what the biopsy results are, will determine whether further treatment is required.
Useful Websites:
British Sjögren’s Syndrome Association
Revised International Classification Criteria for Sjögren’s Syndrome
Useful Articles
The Laryngoscope 2009. The Minor Salivary Gland Biopsy as a Diagnostic Tool for Sjögren’s Syndrome.
Minor Salivary Gland Biopsy
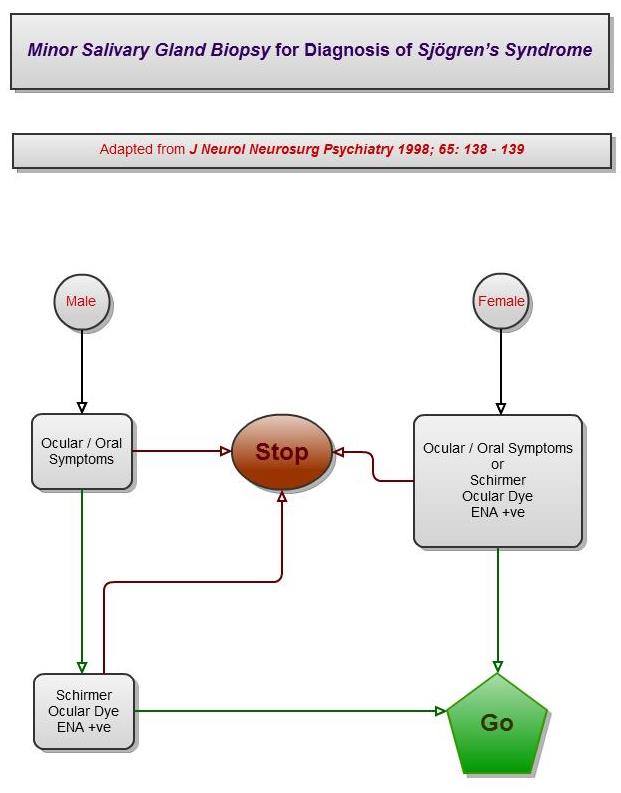
In suspected cases of Sjögren’s Syndrome, patients are often referred for a lower lip minor salivary gland biopsy.
The minor salivary gland biopsy by itself will not diagnose time the biopsy happens, the patient would have already had a number of other clinical, blood, functional and morphological investigations [as laid out by the American-European Consensus Group]).
Biopsy of the minor salivary glands of the lower lip has been used for many years as the changes in the lower lip mirror those in the major salivary glands (parotid and submandibular glands). The presence of chronic inflammatory cells in lip salivary glands, as assessed with the minor salivary gland biopsy, is one of the parameters included in most criteria sets proposed for Sjögren’s Syndrome classification.
What is a Minor Salivary Gland Biopsy & How Is It Done?
A Minor Salivary Gland biopsy is a procedure where an incision is made within the lower lip and minor salivary glands present just below the surface are plucked out and looked at closely under a microscope. It is a relatively minor and safe procedure.
A local anæsthetic injection is used to numb the area which takes a couple of minutes to work. After this injection, the procedure should be painless. An incision, needing stitching afterwards, is made to the lower lip. The stitches dissolve after 10 – 14 days. All together, this procedure usually takes around 15 – 20 minutes from start to finish.
Is there much soreness afterwards?
When the anæsthetic wears off, there will be some pain and discomfort. Simple painkillers will usually be effective. You will be advised which are the best to take. Any discomfort usually only lasts a few days.
Will there be much bleeding?
Although there may be a little bleeding at the time of the biopsy, this usually stops very quickly and is unlikely to be a problem if the wound is stitched. When you get home, should the biopsy site bleed again, apply pressure over the area for at least 10 minutes with a rolled up handkerchief or swab (if you have been given one). This should stop the bleeding but if the bleeding continues please contact your Oral Surgeon / OMFS Department.
When can I return to work?
This largely depends on your job and how you feel after the procedure. Most people are able to return to work later the same day.
Will I need another appointment?
A follow-up appointment is not always necessary but you will usually be asked to attend an appointment for the results of the biopsy to be discussed with you. A care advice leaflet will be given to you after the biopsy.
Minor Salivary Gland Biopsy – Operation Warnings
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004] [https://exodontia.info/chester-vs-afshar-2004/], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
The following list of warnings regarding minor salivary gland biopsies is neither exhaustive nor is it predictive.
The most pertinent warnings have been included here.
As it is a surgical procedure, there will be soreness after the procedure. This can last for several days. Painkillers such as ibuprofen or paracetamol are very effective. Obviously, the analgesic you use is dependent on your medical history and the ease with which the biopsy was carried out.
Swelling.
There will be swelling afterwards. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that will develop.
Stitches.
The biopsy site will be closed with stitches. These are dissolvable and & will “fall out” within 10 – 14 days.
Scarring / Lumpiness at Biopsy Site.
Any cut to soft tissues produces a scar. Initially, after a biopsy, a scar will be produced. This softens and disappears (i.e. improves) with time. Regardless, it can feel quite obvious and lumpy to begin with. The scarring can also dependent on the size and size of the biopsy and the individual’s tendency to scarring.
Initial Tautness / Tenderness at Biopsy Site.
To close the biopsy site, the wound margins are closed with stitches. These place tension and hence tenderness at the biopsy site; this tails off with time.
Localised Area of Numbness at Biopsy Site.
The biopsy can damage the local nerves resulting in areas of numbness. These can take a number of months before normal feeling returns.
Inconclusive Results & the Need for Re-biopsy.
The biopsy results can come back as inconclusive. If this is the case, then it is possible that the biopsy will need to be repeated.
Further treatment dependent on Results.
Depending on what the biopsy results are, will determine whether further treatment is required.
Useful Websites:
British Sjögren’s Syndrome Association
Revised International Classification Criteria for Sjögren’s Syndrome
Useful Articles
The Laryngoscope 2009. The Minor Salivary Gland Biopsy as a Diagnostic Tool for Sjögren’s Syndrome.