Inferior Dental (Alveolar) & Lingual Nerve Injuries
The (surgical) removal of lower wisdom teeth (3rd molars) endangers both the lingual and inferior alveolar nerves; as the removal of (lower) potential number of patients sustaining nerve damage is likewise high.
The majority of injuries result in transient sensory disturbance but, in some cases, permanent abnormal sensation (paræsthesia), reduced sensation (hypoæsthesia) or, even worse, some form of unpleasant abnormal sensation (dysæsthesia) can occur.
These sensory disturbances can be troublesome, causing problems with speech and chewing and may adversely affect the patient’s quality of life.
They also constitute one of the most frequent causes of complaints and litigation.
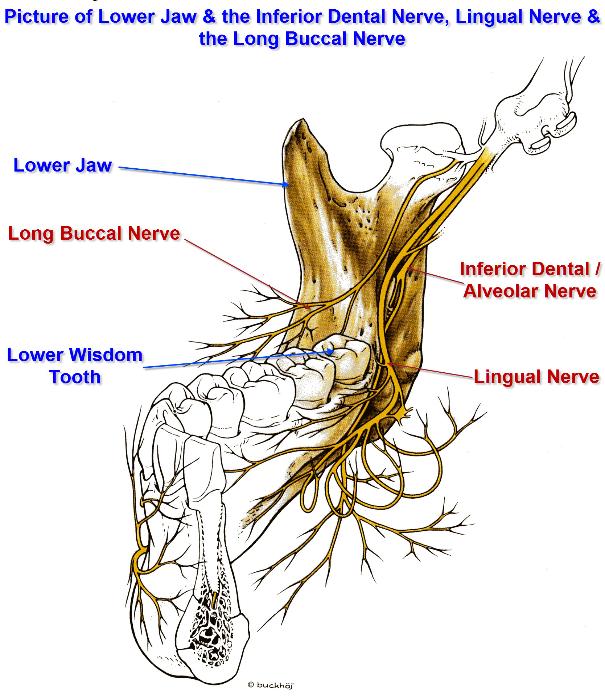
As can be seen from the illustrations below, branches of the Mandibular Nerve (the third and lowermost division of the Trigeminal Nerve or the 5th Cranial Nerve) can be in close proximity either to the roots of the wisdom teeth (also the 2nd molars as well) or to either side of the tooth crown.
The branches of the Mandibular Nerve that are of significance to wisdom teeth removal, include the:
- Inferior Alveolar (or Inferior Dental) (IAN / IDN)
- Lingual (LN)
- Long Buccal (LB)
- Mylohyoid (MH)
- Mental (MN)
Hence, trauma to these nerves can result in either numbness, tingling, altered sensation or a loss of taste (or a combination Trauma, here, covers stretching, crushing or cutting of these nerves. The degree of trauma will greatly determine the degree of numbness (and loss of taste) and its duration. Trauma can be due to use of instruments to remove the tooth, drills used to remove bone and ‘elevators’ used to ‘protect’ the LN.
Trauma to the LN & the IAN can also result from the injection of local anæsthetic (some local anæsthetics have been found to cause prolonged numbness), fracture of the Lingual Plate, jaw fractures, osteotomies for the correction of malocclusion and the removal of pathology in proximity to the IAN or the LN (such as peeling a dentigerous cyst out of its cavity).
As this is a well recognised complication of lower wisdom tooth removal, patients need to be warned about the potential for numbness (temporary / permanent) prior to surgery so that the patient can weigh up the pros & cons and the potential consequences of the procedure and if needs be, opt for a different surgical treatment (such as a coronectomy or operculectomy).
Before the removal of the wisdom tooth (in fact, any teeth), the mouth needsto be assessed radiographically (i.e. X-rayed).
This, amongst other things, will show whether the IAN canal is in proximity to the wisdom tooth and there are certain appearances on the OPG that suggest the IAN canal is intimate with the tooth.
Studies have shown that these aren’t always reliable and the definitive information can be gained with a Cone Beam CT scan (now becoming routinely used).
The spontaneous recovery rate for nerve injuries related to lower wisdom tooth (3rd molar) removal is quite variable ranging from 50% – 100% for both the IAN and LN.
Incidence of Nerve-Damage relating to Wisdom Tooth Removal:
Inferior Alveolar Nerve. IAN function is disturbed in 4 – 5% of procedures (range 1.3 – 7.8%). Most patients will regain normal sensation within a few weeks or months and < 1% (range 0 – 2.2%) have a persistent sensory disturbance.
A higher incidence of IAN injury has been reported with wisdom teeth that are horizontally or mesio-angularly impacted and have complete bone cover.
One study has also demonstrated that increasing age is associated with a higher frequency of IAN injury (14 – 24 year old patients 1.2%; 35 – 81 year-old patients, 9.7%).
Lingual Nerve. There is a wide range in the reported frequency of LN injuries during lower wisdom tooth, with 0.2 – 22% of patients reporting sensory disturbances in the early post-operative period and 0 – 2%, a permanent disturbance.
A higher incidence of IAN injury has been reported with certain types of surgical technique (using an ‘elevator’ to ‘protect’ the LN) together with deeply impacted teeth when the surgery is consequently difficult, particularly if distal bone removal is required.
Most cases of nerve damage during wisdom tooth removal are not identified at the time of lower wisdom teeth removal but in the post-operative period.
However, careful monitoring of sensory recovery over a three month period should distinguish between these different types of injury.
Monitoring sensory recovery is undertaken by the application of stimuli to the ‘numb’ area. Responses of the patient will indicate first the arrival of the regenerating nerve ends and then subsequently the level of recovery.
However, the most sensitive indicator of a sensory abnormality is the patient’s own subjective report, as minor sensory disturbances may not be detected by testing.
Simple Sensory Testing
A standard protocol for sensory testing does not exist and attempts to standardise objective evaluation of nerve injuries have been unsuccessful.
Evaluation techniques are subjective or semi-objective at best.
Suggested techniques include:
Mapping out and photographing the area involved
Light touch is most commonly tested by gently applying a wisp of cotton wool to the skin or lining of the cheek or lips.
However, it is difficult to apply this stimulus in a reproducible manner and the use of a cotton wool wisp on moist oral mucosa is difficult.
Greater consistency and reproducibility can be obtained using Von Frey hairs. Stimuli are applied at random and the area of anaesthesia can be stimulus is felt.
Pin Prick Sensation
Testing pin prick threshold is often performed using a dental probe or needle but reproducibility is poor. Areas of anæsthesia can be mapped. If sensation is present within the affected area on the injured side, then the pin prick sensation threshold is determined.
The probes are drawn a few millimetres across the surface, at a constant pressure and the patient asked to indicate the point at which the sensation becomes sharp rather than dull.
The pin prick sensation threshold is noted for a series of randomly chosen points on both the ‘injured’ and the ‘uninjured’ side.
Two Point Discrimination
This test can quickly be performed if pairs of blunt probes with different separations (2 – 20 mm) are mounted around a disc.
The probes are applied at a series of fixed sites chosen on the lips or tongue, depending on which has been damaged.
The probes are drawn a few millimetres across the surface, at a constant pressure and the patient is asked whether one or two points are felt. The minimum separation, that is consistently reported as two points, is termed the two point discrimination threshold.
This threshold varies in different regions of the mouth (2 – 4 mm on the tongue and lip, 8 – 10 mm on the skin over the lower border of the chin).
Taste Stimulation
Cotton wool pledgets soaked in saline solution, sugar solution, vinegar or quinine solution are drawn 1 – 2 cm across the side of the tongue and the patient asked to indicate whether they taste salt, sweet, sour, bitter or no taste, before Stimuli should be applied in random order, to each side of the tongue and rinsing with tap water between tests.
The most desirable outcome after nerve injury is the spontaneous return of normal sensation.
The likelihood of this occurring depends on both the severity of the injury and the nerve involved.
Inferior Alveolar / Dental Nerve:
If a sensory disturbance is first noted at review, recovery should be monitored using the sensory tests described above.
Patients with paræsthesia in the distribution of the IAN (evoked by touching the lip or chin) usually require no surgical intervention.
Patients with complete anæsthesia post-operatively should be evaluated radiographically (such as an OPG or a CT scan) to ensure that the roof of the nerve canal has not been displaced downwards to create an obstruction to nerve repair and regeneration. In the extremely rare event that this has occurred, removal of the bony fragment would seem to be appropriate, without undue delay.
Referral to an Oral & Maxillofacial surgeon familiar with this type of procedure or a neurosurgeon or a micro-neurosurgeon is important. The patient should know that full recovery may not be achieved even with surgery though some recovery may occur even if surgical ‘decompression’ is not performed.
If, after 3 months after the injury, monitoring reveals little or no sensory recovery, referral is again indicated. A further X-ray to assess the continuity of the IDN canal is obtained and surgical exploration and ‘decompression’ of the nerve is considered if the canal is disrupted, if there is very little recovery of sensation or if there is significant dysæsthesia.
However, the results of surgery are variable and sometimes disappointing.
Lingual Nerve:
If the LN is knowingly cut during wisdom tooth removal, it should be immediately repaired.
This may not be possible in dental practice and immediate referral to an appropriate experienced Oral & Maxillofacial surgeon is indicated. In the majority of patients, the injury is only discovered post-operatively.
At early review, the presence of some sensation in response to stimulation of the tongue suggests that the nerve is at least partially intact; no treatment is indicated but sensory monitoring is required.
Complete anæsthesia could be caused by both a crush or cutting injury and so surgical intervention is not indicated initially.
However, the absence of progressive sensory recovery by 3 – 4 months post-injury is an indication for surgical exploration at an appropriate Oral & Maxillofacial unit.
If, at the time of surgery, the nerve is found to be intact and of fairly uniform thickness but merely constricted by scar tissue, it should be freed (external neurolysis) and the wound closed. This is unusual however and more commonly the nerve is found to have been cut.
If a neuroma has developed, this can be seen as a marked expansion at the site of the injury and must be removed together with the damaged segment of the nerve. A nerve graft is then used. The results of surgery are very variable; some patients regain good sensation whilst others show little if any improvement.
One study showed a success rate of 80% and a recent prospective study has shown that the majority of patients consider the surgery worthwhile. Surgery should therefore be offered to all patients with LN injury who show few signs of spontaneous recovery.
Useful Contact Addresses:
In the UK (at the moment, I can only find the details for England), there are seemingly 2 major centres regarding ‘dental nerve’ injuries; these are based at the King’s Dental Institute, London and at the School of Clinical Dentistry, Sheffield.
If you want to contact them about being seen regarding your nerve injuries, they can be emailed at the following email addresses; Professor Renton (King’s) and Mr Simon Atkins (Sheffield).
Useful Articles & Websites
University of Sheffield, School of Clinical Dentistry
BJOMS 1990. A method of assessment in cases of lingual nerve injury
BJOMS 1992. Experiences in Lingual Nerve Repair
Braz J Oral Sci 2003 – Evidence Based Means of Avoiding Lingual Nerve Injury
Dental Update 2003 – Nerve Damage and Third Molar Removal
JADA 2003 – Lingual Nerve Damage due to inferior alveolar nerve blocks – A possible explanation
BJOMS 2005 – Objective evaluation of iatrogenic lingual nerve injuries using jaw-opening exercises
JOMS 2005. Frequency of Trigeminal Nerve Injuries following 3rd Molar Removal
JOMS 2005. Diagnosis and Management of Trigeminal Nerve Injuries
JOMS 2005. Lingual Nerve Damage After Mandibular Third Molar Surgery – A Randomized Clinical Trial
JOMS 2005. The Effect of Injury and Protocols for Management
JOMS 2005. The Results of Nerve Repair and the Management of Nerve Injury–Induced Pain
BDJ 2006 – Simplifying the assessment of the recovery from surgical injury to the lingual nerve
JOMS 2006. Frequency & Evolution of Lingual Nerve Lesions Following Lower 3rd Molar Extraction
JOMS 2006. Late Surgical Management of Lingual Nerve Injuries – Outcome Assessment
JOMS 2006. Etiology of Lingual Nerve Injuries in the 3rd Molar Region – A Cadaver & Histologic Study
JOMS 2006. Outcome Assessment of Inferior Alveolar Nerve Microsurgery – A Retrospective Review
JOMS 2007. Functional Sensory Recovery After Trigeminal Nerve Repair
CDAJ 2007 – Permanent Nerve damage from IAN Blocks – An Update to include Articaine
Cochrane Collaboration 2008 – Interventions for Iatrogenic IAN Injury (Protocol)
Oral Surgery 2008 – IAN decompression and neurolysis
BDJ 2010. Trigeminal Nerve injuries in relation to the local anaesthesia in mandibular injections
Faculty Dent J 2011. Minimising and managing nerve injuries in dental surgical procedures
JOMS 2011. Long-Term Outcome of Trigeminal Nerve Injuries Related to Dental Treatment
Cochrane Review 2014. Review. Interventions for Iatrogenic Inferior Alveolar & Lingual Nerve Injury
Dental Update 2018. Trigeminal Nerve Injuries Related to Restorative Treatment