What is Dry Mouth?
What is Dry Mouth?
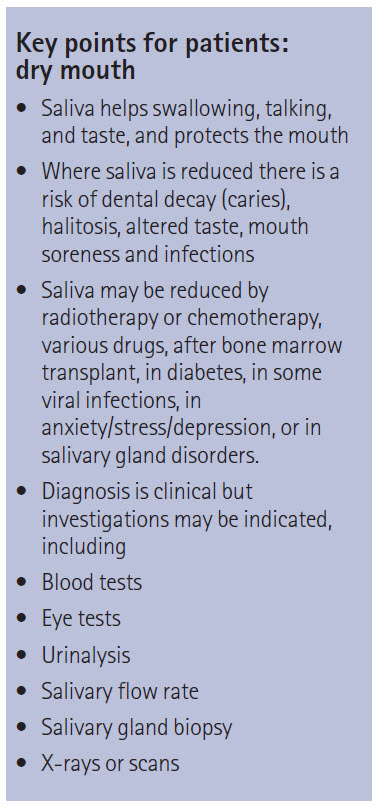
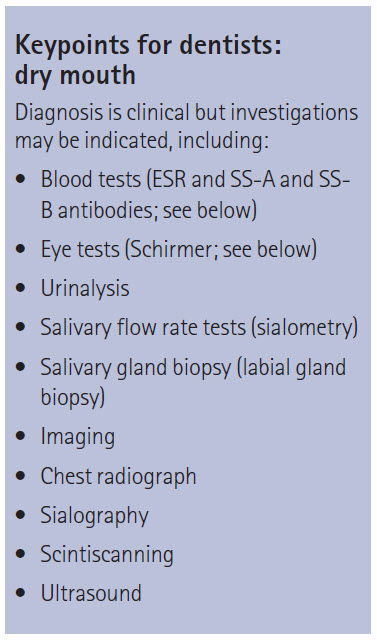
Dry Mouth or Xerostomia is not a disease in itself, but can be a symptom of certain diseases.
It can negatively affect a patient’s quality of life-impacting on eating habits, nutritional health, speech, taste, tolerance to dental prosthesis (such as dentures) and can increase the likelihood of dental decay.
What are the causes of Dry Mouth?
[link to Causes of Dry Mouth webpage]
Dry Mouth can result from a number of causes, such as the use of certain drugs (such as anti-hypertensives, tricyclic anti-depressants, analgesics, tranquilizers, diuretics and anti-histamines); inflammatory conditions such as Mumps, TB, Sarcoidosis and Sjögren’s Syndrome; obstructions such as salivary stones; conditions such as dehydration, diabetes, cardiac and renal failure, toxic goitre, menopause and senility; nutritional causes such as Vitamin A and iron deficiency; cancer treatment such as chemotherapy and radiotherapy and psychiatric causes.
What can be done to relieve Dry Mouth?
- The lack of saliva can have a profound effect on the mouth and the teeth.
- There are a number of things you can do to relieve the symptoms:
Sip / drink water frequently. - Stimulate saliva with sugar-free gum (such as Xylitol), diabetic sweets, Salivix or SST if advised.
- Keep your mouth clean, paying special attention to the teeth.
- Use an artificial saliva (Artificial Saliva, Glandosane, Luborant) or saliva substitute (such as Orthana or Oral Balance-Biotène).
- Use an antiseptic mouthwash (such as Corsodyl or Biotène).
- Avoid alcohol-based mouth rinses.
- Spray a water and glycerine solution into your mouth, mixed in a small aerosol bottle.
- Always take water or non-alcoholic drinks with meals.
- Avoid anything that worsens the dryness, such as certain drugs (see above), alcohol, smoking, caffeine and mouth-breathing.
- Protect against dental decay by using a Fluoride mouth rinses / gels (such as Fluorigard), regular dental checks, avoiding sugary foods / drinks and sticky food.
- Protect against Thrush & Halitosis by your mouth very clean and moist, rinsing twice daily with chlorhexidine (Corsodyl, Chlorhex or Eludril) or Triclosan (Plax), brushing or scraping of tongue, keeping dentures out at night and soaked in hypochlorite (eg Miltons or Dentural) and use of anti-fungals (if prescribed by your clinician).
- Protect the lips with a lip salve or petroleum jelly (eg Vaseline).
Consider a humidifier in the room.
You can also make dietary changes to help the condition – blended and mixed foods are easier to swallow.
Eat hard cheeses instead of soft cheeses and use sucralose in place of sugar. Avoid spicy, hard crunchy or dry foods. Take small bites and eat slowly. Pineapple has an enzyme that helps clean the mouth.
Drugs such as pilocarpine or cevimeline are sometimes prescribed but these drugs have many side effects that many people can not tolerate.
(Adapted from the Eastman Dental Institute, Oral Medicine Clinic – Dry Mouth – 10 steps towards managing a dry mouth. My thanks to Prof Scully for updating me regarding this).
Useful Articles & Websites
Biotène products available from www.biotene.co.uk
Xerotin products available from www.SpePharm.com
BioXtra products available from www.bioxhealthcare.com
Aquoral products available from www.aquoral.com
Table comparing the various saliva substitutes & preparations used to treat dry mouth / xerostomia
British Sjögren’s Syndrome Society
Sjögren’s Syndrome Online Community
American Dental Association – Dry Mouth
Eastman Dental Institute, Oral Medicine Clinic – Dry Mouth – 10 steps towards managing a dry mouth
Eastman Dental Institute, Oral Medicine Clinic – Dry Mouth Patient Information Sheet
Oral Diseases 2002. Current Issues in Sjögren’s Syndrome
Oral Diseases 2002. Drug Effects on Salivary Glands – Dry Mouth
JADA 2007. For The Dental Patient…Oral Moisturizers. Products that can help relieve Dry Mouth
Vital, Spring 2009, Managing Xerostomia
BDJ 2012. Sjögren’s Syndrome; An Update for Dental Practitioners
Dental Update 2012. Oral Medicine 4. Dry Mouth & Disorders of Salivation
Prim Dent J 2015. Dry Mouth & Sjögren’s Syndrome – An Overview
Singapore Dent J 2015. Dry Mouth – An overview
AFP 2016. Dry Mouth – Xerostomia & Salivary Gland Hypofunction
Dent Update 2016. Antimuscarinics in Older People – Dry Mouth and Beyond