Oral Cancer – Ætiological Factors
More than 90% of Oral Cancer is Oral Squamous Cell Carcinoma (OSCC).
OSCC accounts for approx 2 – 4% of all cancers in the UK but is one of the most common cancers on the Indian subcontinent.
Men are more frequently affected than women; most OSCC patients > 40 and the incidence of rises rapidly with age.
The lower lip is the most common site & related to actinic (sun / solar) damage.
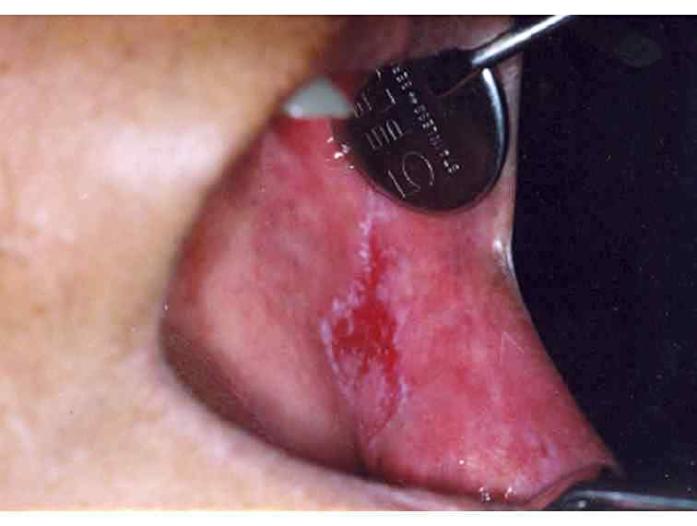
The tongue (the sides especially further back [postero-laterally]), is the most common site within the mouth.
Heavy tobacco smoking & alcohol consumption tend to be associated with the development of OSCC; in India & SE Asia, betel & areca nut chewing may be more important.
 The majority of OSCC involves the lateral border of tongue ± Floor of Mouth. Why are these sites predisposed to tumour development? Perhaps carcinogens pool in saliva in the so called ‘graveyard’ or ‘coffin’ area and there is increased permeability to these chemicals in these areas.
The majority of OSCC involves the lateral border of tongue ± Floor of Mouth. Why are these sites predisposed to tumour development? Perhaps carcinogens pool in saliva in the so called ‘graveyard’ or ‘coffin’ area and there is increased permeability to these chemicals in these areas.
Ætiological Factors for Oral Cancer
Carcinogens
- Tobacco
- Alcohol
- Areca nut / betel
Sunlight (lip only)
Infections
- Syphilis (Syphilitic leukoplakia)
- Candidiasis (Candidal leukoplakia)
- Viruses (HPV)
Mucosal Diseases
- Dysplastic lesions
- Oral Lichen Plamus
- Oral Sub-Mucous Fibrosis
Genetic Disorders
- Dyskeratosis congenita
- Fanconi’s anæmia
 Tobacco
Tobacco
 Alcohol
Alcohol
 Areca Nut / Betel
Areca Nut / Betel

Syphilis (Syphilitic Leukoplakia / Glossitis)
Syphilitic leukoplakia, especially of the tongue dorsum is a feature of tertiary syphilis (rarely seen now) but the malignant potential is high.
Carcinoma developing near the centre of the tongue dorsum is typically the sequel to syphilitic leukoplakia. Given the decline in late-stage syphilis, it is exceedingly rare in this site now.
Candida (Candidal Leukplakia)
leukoplakias especially at the commissures.
It may be associated with an increased risk of malignant change.
Candidal Leukoplakia responds well to anti-fungals & the cessation of smoking. The tongue dorsum is also a common site.
Human Papilloma Virus 16 (HPV 16)
HPV related cancers appear to occur on the tonsillar area, the base of the tongue and the oro-pharynx (non-HPV positive tumours tend to involve the anterior tongue, floor of the mouth, the mucosa that covers the inside of the cheeks and alveolar ridges).
In general, it appears that HPV-positive tumours occur most frequently in a younger group of individuals than tobacco-related malignancies. They occur more in white males and in non-smokers. The HPV-positive group is the fastest growing segment of the oral cancer population.
It does not appear that the HPV 16 acts synergistically with tobacco or alcohol and represents a completely unique disease process.
Oral Lichen Planus
It is estimated that 1 – 4% of patients develop carcinomata after a decade. Plaque-like & erosive OLP in unusual sites (such as the fauces & tongue) should be regarded with suspicion.
In view of the commonplaceness of OLP, its importance as a pre-malignant lesion may be considerable.
Cutaneous LP appears to carry no risk of malignant change.
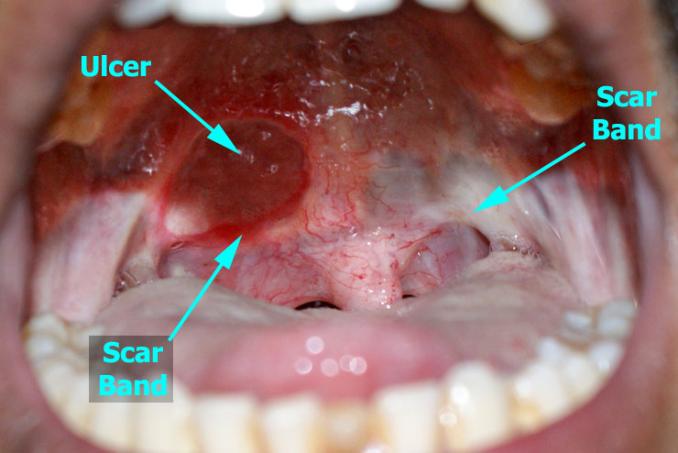
SMF affects those from the Indian sub-continent & SE sclerosis but limited to the oral tissues & without the immune abnormalities.
Arecoline, a stimulant derive from the areca nut is thought to induce fibroblast proliferation & collagen synthesis.
Clinically, there is symmetrical fibrosis (scarring) of the buccal mucosæ, soft palate & the inner aspects of lips.
The overlying mucosa may be normal or there may be a vesiculating stomatitis. Fibrosis & ishæmia causes extreme pallor of the affected area which becomes so hard that it can’t be indented by your finger.
Progressive trismus making it very difficult to eat / drink. Malignant change is from 4.5 – 8 %.

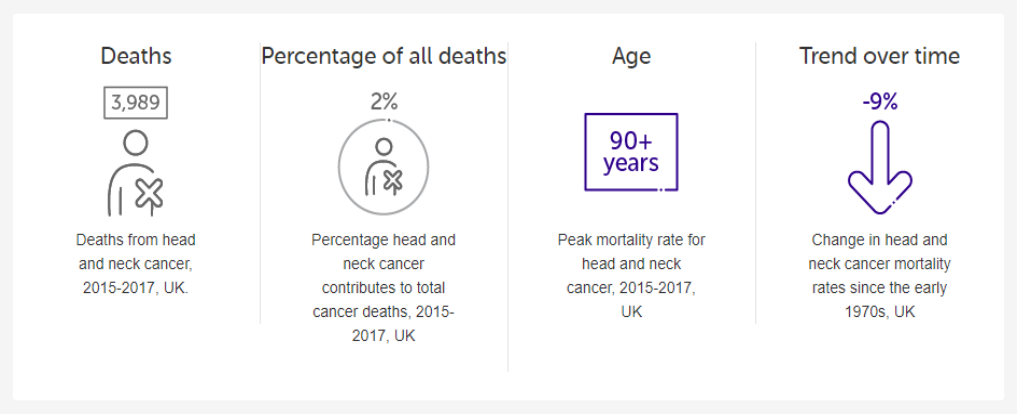
 National Statistics for Head & Neck Cancer in the UK, 2015 – 2017
National Statistics for Head & Neck Cancer in the UK, 2015 – 2017