Oral Mucositis
Oral mucositis refers to erythematous (reddened) and ulcerative lesions of the oral mucosa observed in patients with cancer being treated with chemotherapy and / or with radiation therapy to areas involving the oral cavity.
Oral mucositis is often very painful and can result in odynodysphagia (painful swallowing), dysgeusia (bad taste in mouth) & subsequent dehydration & malnutrition, compromising nutrition and oral hygiene as well as increase risk for local and systemic infection.
Oral mucositis (also called stomatitis, though in this context, it is the diffuse inflammatory, ulcerative condition affecting the mucous membranes lining the mouth), is a common, debilitating complication of cancer chemotherapy & radiotherapy. It results from the systemic effects of cytotoxic chemotherapy agents and from the local effects of radiation to the oral mucosa.
Oral mucositis is inflammation of the mucosa of the mouth which ranges from redness to severe ulceration. Symptoms of oral mucositis vary from pain & discomfort to an inability to tolerate food or fluids.
 Photos of Oral MucositisOral mucositis may also limit the patient’s ability to tolerate either chemotherapy or radiotherapy. Oral mucositis may be so severe as to delay treatment and so limit the effectiveness of cancer therapy.
Photos of Oral MucositisOral mucositis may also limit the patient’s ability to tolerate either chemotherapy or radiotherapy. Oral mucositis may be so severe as to delay treatment and so limit the effectiveness of cancer therapy.
Patients with oral mucositis are also prone to opportunistic infections in the mouth. The patients’ gingival (gums) & dental condition, speech & self-esteem are reduced, further compromising patients’ response to treatment and /or palliative care.
It is therefore extremely important that mucositis be prevented whenever possible or at least, treated to reduce its severity and possible complications.
Oral mucositis typically occurs 7 – 14 days after chemotherapy or radiotherapy and may last for 2-3 weeks after the completion of treatment.
It is important to take preventative measures against oral mucositis and to recognise and treat it promptly and effectively if it occurs.
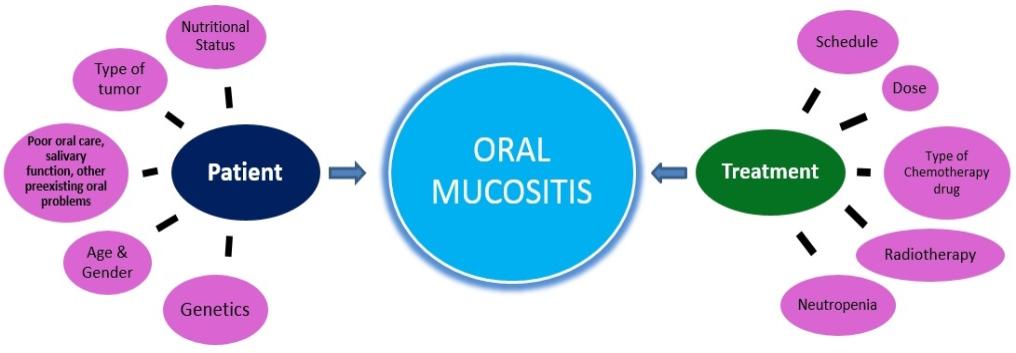
What are the causes of Oral Mucositis?
Treatments most commonly associated with oral mucositis include:
- Anti-metabolites e.g. 5-FU, capecitabine, methotrexate
- Anthracyclines e.g. epirubicin, doxorubicin
- All lymphoma or leukæmia patients who have recently had treatment
- Tyrosine Kinase Inhibitors (such as sunitinib, pazopanib, afatinib) and everolimus
- Radiotherapy to the head & neck region
It is important to take preventative measures against mucositis and to recognise and treat it promptly & effectively if it occurs.
What are the signs & symptoms & how is it diagnosed?
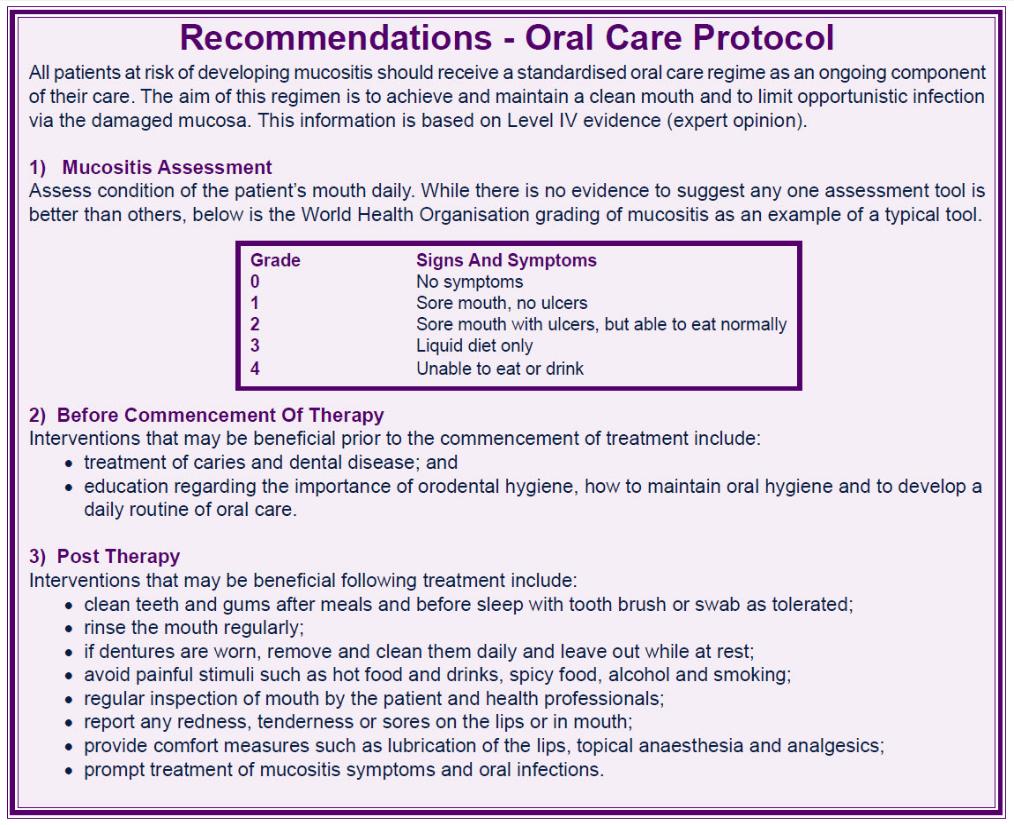
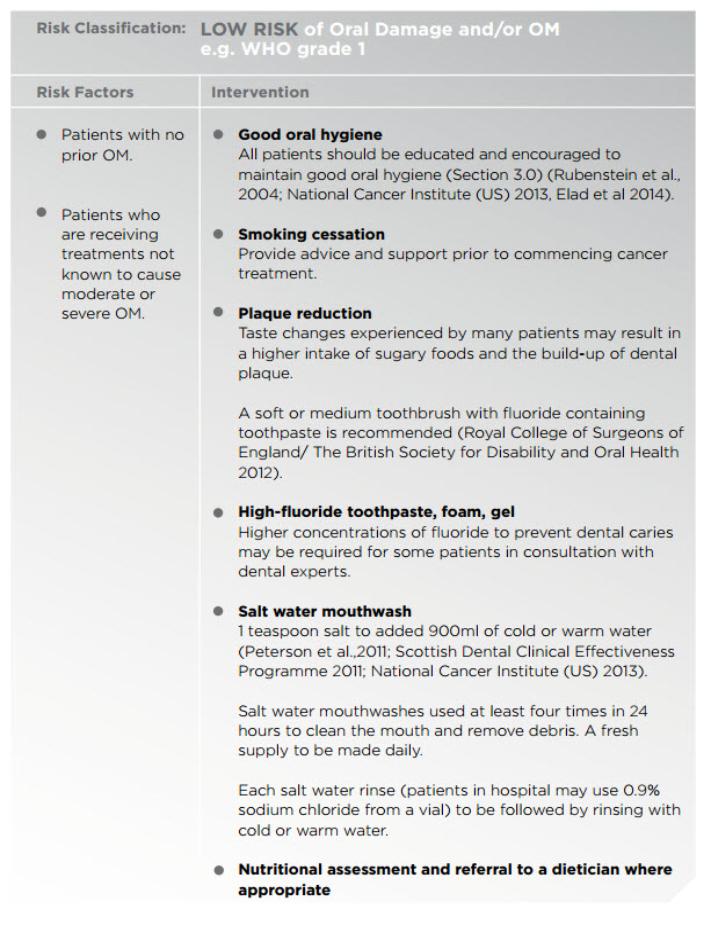
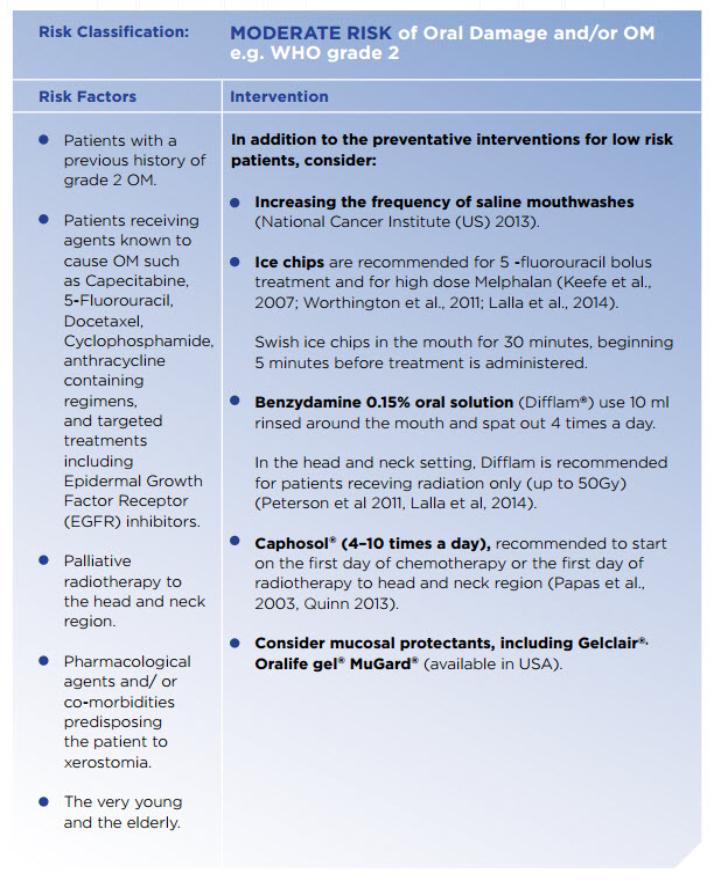
The diagnosis of oral mucositis is based on the symptoms the patient is experiencing and the appearance of the tissues in the mouth following chemotherapy or radiotherapy. The severity of oral mucositis can be evaluated according to several different assessment tools.
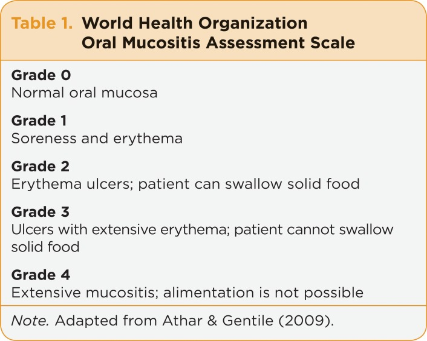
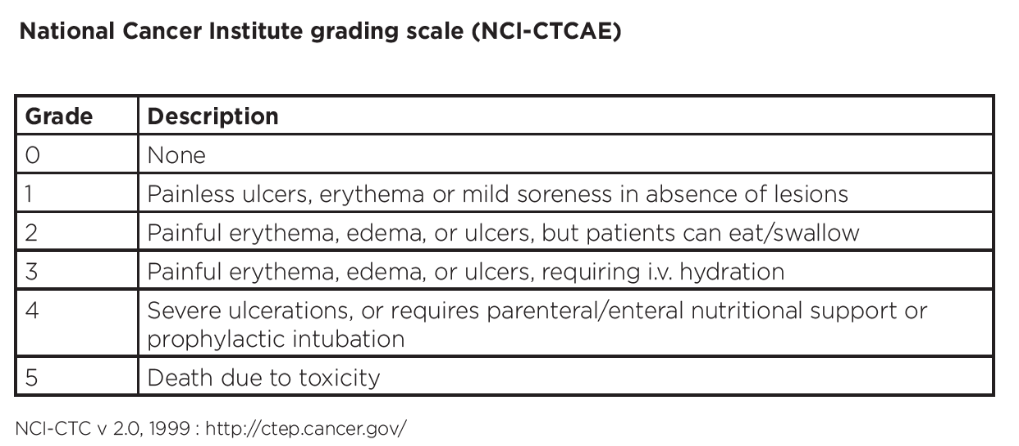
A number of scales are available, including those developed by the WHO, the Radiation Therapy Oncology Group, the Western Consortium for Cancer Nursing Research & the National Cancer Institute (NCI), amongst others.
Two of the most commonly used scales are the WHO Oral Toxicity Scale and the NCI Common Toxicity Criteria for oral mucositis.
While the NCI system has separate scores for appearance (erythema & ulceration) and function (pain & ability to eat solids, liquids or nothing by mouth), the WHO score combines both elements into a single score that grades the severity of the condition from 0 (no oral mucositis) to 4 (swallowing not possible, such that patient needs supplementary nutrition).
How is it treated?
Many different treatments are used to mitigate, possibly prevent or ameliorate the oral mucositis.
Treatment of mucositis is mainly supportive, with both non-pharmacological and pharmacological options.
Non-pharmacological methods include:
Preventive strategies involving a pre-treatment dental examination and improved dental hygiene, since good oral hygiene is the mainstay of treatment. Patients should be encouraged to clean the mouth every 4 hours and at bedtime, and more often if the mucositis worsens. Patients should have the mouth checked regularly, brush the teeth with a gentle toothbrush two or three times daily, use a non-detergent toothpaste, floss between the teeth & use an alcohol-free mouthwash
The use of artificial saliva & water-soluble jellies to lubricate the mouth. Dry-mouth lozenges & dry-mouth gum also may be used (see below)
The use of saline / baking soda mouthwash to soothe the pain & remove food particles to avoid infection
Drinking plenty of liquids – at least 3 litres per day – & avoiding alcohol
Ingested food should be soft, non-spicy, pureed or in liquid form. Harder foods should be treated to make them soft and easy to eat
Refraining from smoking
Sucking ice cubes. This is a simple, but often effective, method of relieving the symptoms of oral mucositis
Text contentPharmacological options include:
Interventions to reduce the mucosal toxicity of chemotherapy drugs (eg allopurinol M/W 4 – 6 x daily & cryotherapy)
Mouthwashes with mixed action (eg benzydamine hydrochloride, corticosteroids & chamomile)
Immunomodulatory agents (eg Granulocyte-Macrophage Colony Stimulating Factor (GM-CSF) & Granulocyte Colony Stimulating Factor (G-CSF))
Topical anaesthetics (eg dyclonine HCl, viscous lignocaine with 1.0 % cocaine & a solution containing kaolin-pectin, diphenhydramine & saline)
Antiseptics (eg Chlorhexidine, Povidone Iodine & Hydrogen Peroxide)
Antibacterial, antifungal & antiviral agents (eg Nystatin, Clotrimazole & PTA lozenges (polymixin E, tobramycin and amphotericin B); Clotrimazole alone, or in combination with Polymixin B & Tobramycin; Acyclovir)
Mucosal barriers and coating agents (eg Sucralfate, sodium alginate, kaolin-pectin, plastic wrap film, radiation guards & antacids)
Cytoprotectants (eg β-carotene (pro-vitamin A), Vitamin E, Oxpentifylline, Azelastine, Prostaglandins E1 & E2)
Mucosal cell stimulants (low energy laser treatment, Silver nitrate, glutamine)
Psychotherapy (Cognitive Behaviour Training, Relaxation & Imagery Training, Hypnosis & Therapist Support)
Analgesics (Patient Controlled Analgesia, Alfentanil, Morphine, Capsaicin)
Drugs for dry mouth & artificial saliva
Useful Articles & Websites
American Academy of Oral Medicine
Cochrane Review – Can oral cryotherapy help to prevent chemotherapy‐induced oral mucositis?
Best Practice 1998. Prevention & Treatment of Oral Mucositis in Cancer Patients
Summary of 2004 MASCC Guidelines for the Treatment of Oral and GI Mucositis
Clinical J Oncology Nursing 2005. Current Trends in Managing Oral Mucositis
Dent Clin North Am 2008. Management of Oral Mucositis in Patients with Cancer
Int J Head & Neck Surg 2010. Strategies in Management of Oral Mucositis
Int Dent J Student’s Res 2012. Oral Mucositis – Management Protocol By Oral Physician
J Clin Exp Dent. 2014. Prevention & Treatment of Oral Mucositis in Patients receiving Chemotherapy
Front Oncol 2017. Radiation-induced Oral Mucositis
Int J Mol Sci 2017. Oral Mucositis – Melatonin Gel an Effective New Treatment
J Clin Oncol Oncology Practice 2020. Evidence-Based Management of Oral Mucositis
European Oral Care in Cancer Group Oral Care Guidance & Support. 1st Edition