Oral Cancer – Rôle of GDP in Cancer Prevention & Diagnosis
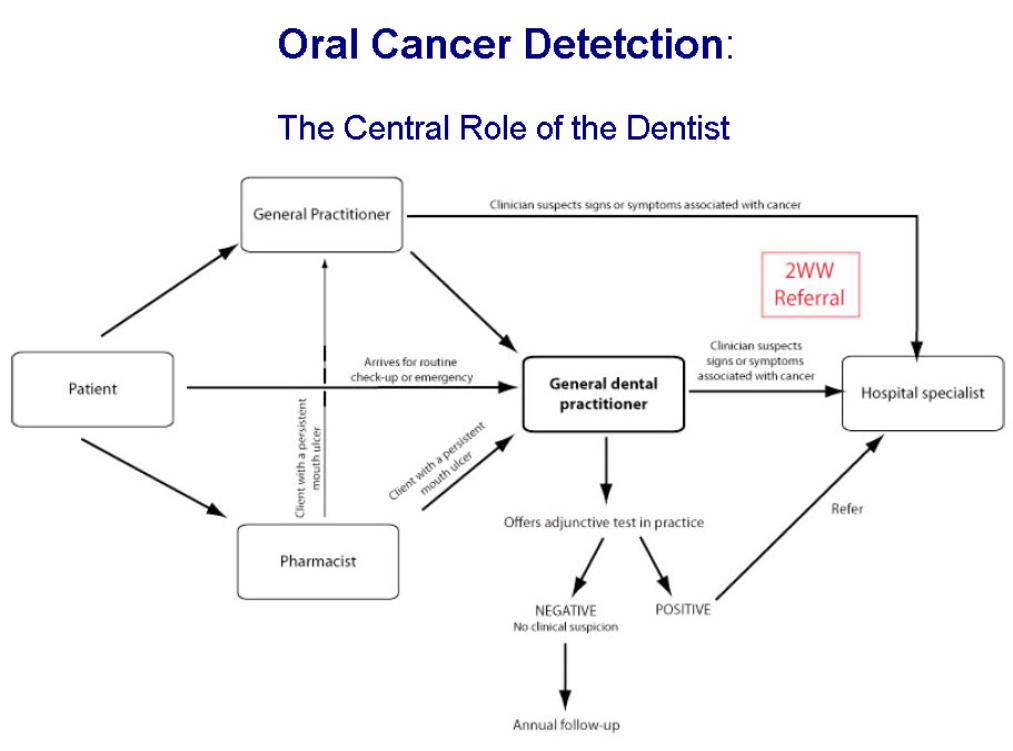
The dentist (GDP) is in a unique position to help in oral cancer discovery and diagnosis.
The GDP, by training and experience, knows what the oral cavity should look like and be aware when oral tissues look suspicious.
GDP’s involvement includes prevention, early diagnosis and the care of patient post-treatment for cancer.
Prevention:
- Actively discourage smoking & betel nut use
- Encourage moderation of alcohol intake
- Health promotion & education on Oral Cancer
- Provide check-ups for œdentulous ± institutionalised elderly & otherwise high-risk non-attenders
Case law has already established that a dentist’s duty of care includes an obligation to examine the whole mouth.
A typical legal complaint might allege failure to recognise the possibility of a malignancy having noted swollen gums and loose teeth, for example, with a lack of evidence of adequate medical and social history taking and delay in making a specialist referral.
Dentists need to be sure that they can, if necessary, answer questions like these:
- Did you know that a particular patient fell into an oral cancer high risk group and what did you do in the light of that knowledge?
- Were the medical, social and dental histories taken appropriately?
- Did you investigate the health of soft tissues thoroughly enough?
- Was a decision not to refer the appropriate one in the circumstances?
- Always examine mucosa as well as teeth
- Refer all high-risk lesions on discovery
- Monitor low-risk pre-malignant lesions
- Perform biopsy appropriately
This presupposes that the GDP is comfortable recognising pre-malignant lesions and is au fait with them. Shrugging your shoulders or referring any oral pathology to the OMFS Department are not necessarily the most efficacious or responsible responses.
Given Continuous Professional Development, there is the expectation that GDP’s should be more aware and be able to recognise oral lesions.
Also, though not happening yet in this country, failure to recognise such lesions and act accordingly may be regarded as malpractice or even negligence.
The parallels have already been drawn by the defence unions between the lack of diagnosis and treatment of periodontal disease and oral cancer.
I don’t believe many GDP’s will biopsy the lesion; no real financial incentives and also the worry that biopsying the lesion may ‘muddy the pitch’ for further investigations and treatment.
- Alleviate the effects of post-irradiation dry mouth (eg preventing xerostomia-related caries)
- Monitor for recurrence, new pre-malignant lesions & second primary tumours
- Monitor for cervical (neck) metastases
- Maintain morale of & provide additional support to patients & their relatives
Theoretically, the GDP should know how to manage a dry mouth and its sequelae (cervical caries, periodontal disease & candidal infections). The GDP should have either literature or even the products used in the amelioration of xerostomia.
If the GDP can do a competent oral screening, than monitoring for a recurrence or a new cancer or a pre-malignancy is no different than the oral screening.
Useful Articles & Websites
Oral Cancer Recognition Toolkit
Br Dent J 2003. The role of primary healthcare professionals in oral cancer prevention and detection
Br Dent J 2003. Oral Cancer Prevention & Detection in Primary Healthcare
BDJ 2010. The Reality of Identifying Early Oral Cancer in the General Dental Practice
BDJ 2012. Oral Cancer – Improving Early Detection & Promoting Prevention. Are you up to date?
Dent Update 2013. Early Detection of Oral Cancer – How Do I Ensure I Don’t Miss a Tumour
BDJ 2013. Why do GDPs fail to recognise Oral Cancer. The Argument for an Oral Cancer Checklist
BDJ 2016. Dentists Can Help Turn The Tide On Oral Cancer
Dent Update 2016. Mouth Cancer for Clinicians Part 9. The Patient & Care Team
Dental Update 2017. Head & Neck Cancer Patients − Information for the General Dental Practitioner
Dental Update 2017. Let’s Talk about Mouth Cancer − The Story & the Facts
British Dental Journal 2018. The Dental Management of a Mouth Cancer Patient
BDJ 2018. Mouth Cancer – Presentation, Detection and Referral in Primary Dental Care
BMJ 2018. Referring patients with suspected oral cancer to dentists may delay diagnosis, say GPs
BDJ In Practice 2020. Oral Cancer – A Ticking Time Bomb
Dental Update 2020. Early Detection of Oral Cancer in General Practice − 30 Years of Searching
Oral Health in Cancer Therapy – A Guide for Health Care Professionals, 3rd edition