Burning Mouth Syndrome
(Glossopyrosis, Glossodynia, Stomatopyrosis, Stomatodynia & Oral Dysæsthesia)
What is Burning Mouth Syndrome (BMS)?
The pain is typically described as burning. It is a persistent and unremitting soreness without aggravating / relieving factors.
It often lasts from months to years.
The intensity of the pain varies from slight to very severe.
Pain-killers seem to have little effect.
There is a bizarre pattern of pain radiation not consistent with the anatomy of blood vessels or nerves. There is sometimes an associated bitter or metallic taste or / and a dry mouth.
This is a common condition. It is not inherited nor is it infectious.
What are its Causes?
Why BMS occurs is uncertain.
It seems to arise from a number of possible causes.
There is no visible abnormality or evidence of organic disease.
BMS is associated with depression, anxiety or a stressful life-situation.
Obsession with symptoms which may rule patient’s life.
Contributing factors may include:
- Thrush infection (thought to be of minor importance)
- Bacterial infections (some antibiotics have been reported to improve BMS)
- Allergies (allergy to denture material)
- Jaw joint problems (thought to be one of the most commonest causes)
- Salivary gland dysfunction (severe dry mouth is thought to be a major cause)
- Deficiencies (in Iron, Folate & vitamin B)
- Hormonal (Diabetes Mellitus)
- Psychological & psycho-social factors seem to play an important role in facial & oro-facial pain.
- Psychogenic factors have been considered as the most common & major causative factors in BMS.
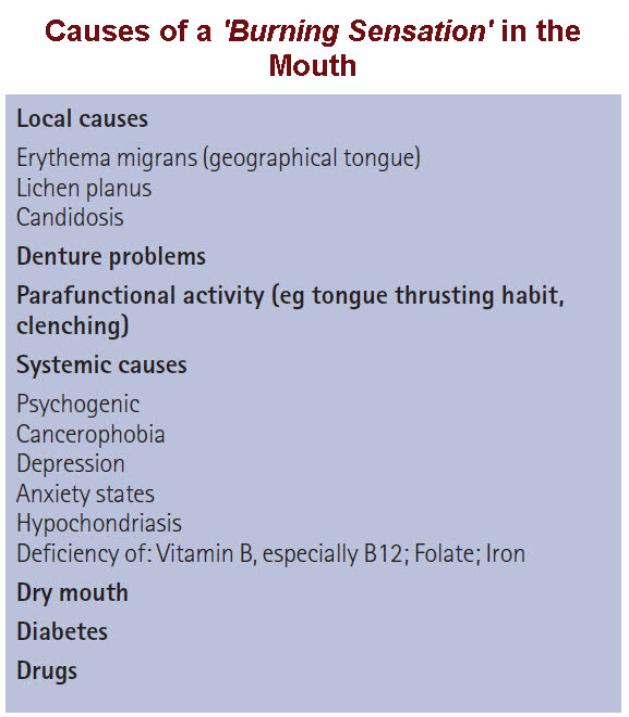 The majority of BMS sufferers have experienced stressful life-events / long-term social problems. After iron deficiency, depression is thought to be the next most frequent causative factor (depression followed by generalised anxiety & cancerophobia).
The majority of BMS sufferers have experienced stressful life-events / long-term social problems. After iron deficiency, depression is thought to be the next most frequent causative factor (depression followed by generalised anxiety & cancerophobia).
In a classification by cause, Idiopathic BMS is considered Primary BMS or True BMS, whereas Secondary BMS has an identifiable cause.
Another classification of BMS is based on symptoms, stratifying cases into 3 types, as follows:
Type 1 BMS: Patients have no symptoms upon waking, with progression throughout the day. Night-time symptoms are variable. Nutritional deficiency and diabetes may produce a similar pattern.
Type 2 BMS: Patients have continuous symptoms throughout the day and are frequently asymptomatic at night. This type is associated with chronic anxiety.
Type 3 BMS: Patients have intermittent symptoms throughout the day and symptom-free days. Food allergy is suggested as a potential mechanism.
BMS is likely more than one disease process and the cause may be multi-factorial. The ambiguous definition of BMS makes evaluation of prognosis and treatment difficult.
Who does it affect?
Middle-aged or older women are mainly affected.
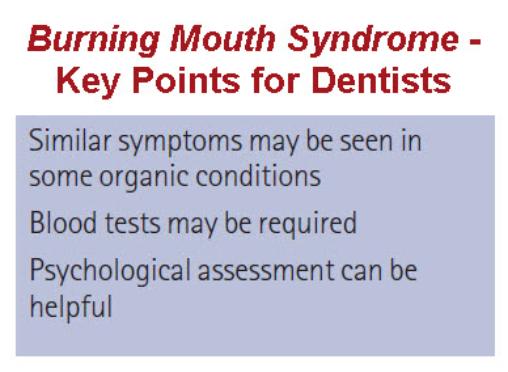
Do I need any special tests?
Yes. As BMS can be due to anæmia, this has to be checked for first however, in a lot of cases, there is no indication of anæmia.
How is it treated?
There is no treatment. Sometimes treatments for thrush can ease the discomfort. If the BMS is due to anæmia, then treatment of the anæmia will help; likewise, if the BMS is related to diabetes.
Mostly though, it is treated as an atypical facial pain; that is, with anti-depressants (though not at a dose where these drugs are acting as anti-depressants). It has been found in small studies, that a food supplement (alpha lipoic acid) has been effective in treating BMS).
Patients often look for constant reassurance and treatment by different practitioners.
 Burning Mouth Syndrome – Diagnosis Algorithm
Burning Mouth Syndrome – Diagnosis Algorithm

Useful Articles & Websites
Pain Res Manage 2003. Burning Mouth Syndrome & other Oral Sensory Disorders – A Unifying Hypothesis
American Dental Association 2005. Burning Mouth Syndrome.
Australian Dent J 2005. Burning Mouth Syndrome. An Update on Recent Findings
Cochrane Collaboration 2005. Interventions for the treatment of burning mouth syndrome
CDA Journal 2007. The Burning Mouth
QJ Med 2007. Commentary. Burning Mouth Syndrome (Stomatodynia)
BMJ Clinical Evidence 2008. Burning Mouth Syndrome
Med Oral Patol Oral Cir Bucal 2008. Burning Mouth Disorder (BMD) & Taste. A Hypothesis
BJOMS 2009. Serum Zinc Levels & Oral Dysaesthesia — Is There A Link?
Clinical Evidence 2009. Burning Mouth Syndrome
J Can Dent Assoc 2011. Management of Burning Mouth Syndrome
J Can Dent Assoc 2011. Diagnostic Dilemma: The Enigma of an Oral Burning Sensation
S Afr Fam Pract 2011. Burning Mouth Syndrome
J Clin Exp Dent 2012. Burning Mouth Syndrome. A Diagnostic & Therapeutic Dilemma
EYAP 2013 Patient Leaflet. Burning Mouth Syndrome
IASP Fact Sheet 2013. Burning Mouth Syndrome
World J Gastroenterol 2013. Burning Mouth Syndrome
J Med Life 2014. Burning Mouth Syndrome – A Review on Diagnosis & Treatment
Cochrane Database of Systematic Reviews 2016. Interventions for treating Burning Mouth Syndrome
Dent Update 2016. Pain Part 8. Burning Mouth Syndrome
Front BioSci 2016. An Overview of Burning Mouth Syndrome
Ind J Pall Care 2016. Burning Mouth Syndrome
J Res Dent Sci 2016. Burning Mouth Syndrome – A Diagnostic Dilemma