Closure of Oro-Antral Communications
This is a common complication, which may occur during an attempt to extract the upper back teeth
or roots (premolars & molars).
The mouth-sinus communication (oro-antral communication) may be confirmed by observing the passage of air or
bubbling of blood from the post-extraction socket when the patient tries to exhale gently through their nose while their
nostrils are pinched (Valsalva test). If the patient exhales through their nose with great pressure, there is a risk of
causing oro-antral communication, even though communication may not have occurred initially, such as when only the
lining (mucosa) of the maxillary sinus is present between the tooth socket and the sinus.
Mouth-Sinus communications (oro-antral communications) may be the result of:
- Displacement of an impacted tooth / root tip into the sinus (maxillary antrum) during extraction.
- Closeness of the root tips to the floor of the sinus (maxillary antrum). The bony portion above the root tips is often very thin or may even be absent, whereupon oro-antral communication is inevitable during extraction of the tooth, especially if the socket is ‘cleaned’ unnecessarily.
- The presence of a root-tip infection (peri-apical lesion) that has eroded the bone wall of the sinus floor.
- Extensive fracture of the maxillary tuberosity, whereupon part of the maxillary sinus may be removed together with the maxillary tuberosity.
- Extensive bone removal for extraction of an impacted tooth / root.
- Apicectomies of maxillary premolars & molars
- Plunging an elevator through the bony floor during root tip removal
- Forcing root tips or tooth into sinus
- Perforation during incorrect curettage
- HIV-associated periodontitis complicated by necrotising stomatitis & the development of an oro-antral fistula
- Enucleating dental maxillary cysts where the partition twixt cyst & antral lining has become blurred
As a very broad generalisation, the following may be thought to indicate an OAC-likely situation:
- Proximity of the Maxillary Sinus / Antrum
- Hyper-cementosis / Ankylosis
- Peri-apical infections / Long-standing Caries (decay)
- Marked Periodontitis (gum disease)
- Proximity to the Tuberosity
- Lone-standing / End of Arch
- Previous history of OAC’s
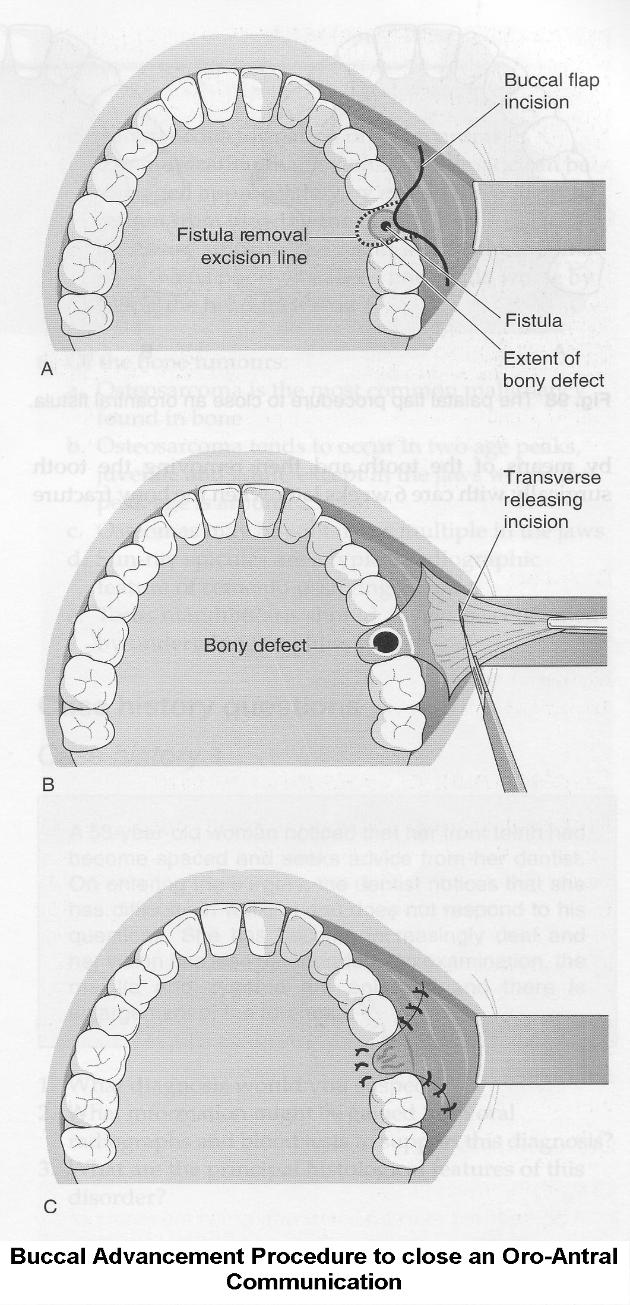
Buccal Flaps
- Buccal Advancement Flap most common (see diagram below).
- Described by Rehrmann & made popular by Berger.
Palatal Flaps
- Palatal Rotational Advancement Flap most common (see diagram below).
- Others include Palatal Pedicle Island Flap (Henderson),
- V-shaped Palatal Flap (Krueger) &
- Split-Thickness Palatal Flap (Ito & Hara).
 The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
Not all possible complications or risks can be foreseen in any medical or surgical treatment, and this is the case for the closure of OAC / OAF’s. There may be other unusual risks that have not been listed here. Please ask your Oral Surgeon if you have any general or specific concerns.
Less Common Surgical Consequences:
Bleeding into Cheeks.
Swelling that does not resolve within a few days may be due to bleeding into the cheek. The cheek swelling will feel quite firm. Coupled with this, there may be limitation to mouth opening and bruising. Both the swelling, bruising and mouth opening will resolve with time.
Breakdown of the Flap & Recurrence of the OAC / OAF.
The flap used to close the mouth sinus hole can breakdown for a number of reasons. If this happens, then, depending on the size of the mouth-sinus hole, the procedure will need to be done again.
Post-op Régime
- Antibiotics (Amoxycillin, Doxycycline)
- Analgesics<
- Steam inhalations (Menthol & Eucalyptus)
- Antiseptic mouth-wash (Corsodyl)
- No nose-blowing or smoking
Common Surgical Consequences:
Pain.
As it is a surgical procedure, there will be soreness after the operation. This can last for several days. Painkillers such as Ibuprofen, Paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history & the ease with which the operation was carried out.
Swelling.
There will be swelling afterwards. This can last up to a week. Use of an icepack or a bag of frozen peas pressed against the cheek adjacent to the operation site will help to lessen the swelling. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling as well.
Bruising.
Some people are prone to bruise. Older people, people on aspirin or steroids will also bruise that much more easily. The bruising can look quite florid; this will eventually resolve but can take several weeks (in the worst cases).
Stitches.
The operation site will be closed with stitches. These are dissolve and ‘fall out’ within 10 – 14 days.
Mouth Opening.
Often the chewing muscles and the jaw joints are sore after the procedure so that mouth opening can be limited for the next few days. If you are unlucky enough to develop an infection afterwards in the socket, this can make the limited mouth opening worse and last for longer (up to a week).
Post-op Infection.
You may develop an infection in the operation site. This tends to occur 2 – 4 days later and is characterised by a deep-seated throbbing pain, bad breath and an unpleasant taste in the mouth. This infection is more likely to occur if you are a smoker, are on the Contraceptive Pill, on drugs such as steroids and if bone has to be removed to facilitate the closure of the oro-antral communication. If antibiotics are given, they are likely to react with alcohol and / or the Contraceptive Pill (that is, the ‘Pill’ will not be providing protection).
BIPP Pack / Coe-Pack Dressing.
When a palatal flap is used, the bone in the roof of the mouth can be exposed. This is sore and can be slow to heal. With this in mind, a dressing (Coe-Pack) or gauze soaked in an antiseptic (BIPP Pack) is sewn over the bare bone to facilitate healing. This is removed 7 – 14 days after the op.
Flattening of Vestibulum (Sulcus).
If the tissue used to close the mouth-sinus hole is drawn from the cheek, then the space between the cheek / lips and the teeth (sulcus) is lessened (temporarily). This tends to slacken off with time but may necessitate a further op to restore the sulcus.
Useful Articles & Websites
BJOMS 1986. Oro-Antral Fistulae – A Study of Clinical, Radiological & Treatment Aspects
Acta Stomat Croat 2002. Treatment of Oro-Antral Fistula
Swiss Med Wkly 2003. The reconstruction of oral defects with buccal fat pad
Turk J Med Sci 2004. Buccal Corticotomy for Closure of Oro-Antral Openings – Case Report
JOMS 2009. Closure of Oroantral Communications with Bichat’s Buccal Fat Pad
JSCR 2010. Oro-Antral Fistula from Bisphosphonates-Induced Osteonecrosis of the Jaw
JOMS 2010. Closure of Oroantral Communications – A Review of the Literature
Med Oral Patol Oral Cir Bucal. 2010. Oroantral Communications. A Retrospective Analysis
Pakistan Oral & Dent J 2010. Treatment of Oroantral Fistula & A Study
BDJ 2011. Oro-Antral Fistulae & Fractured Tuberosities
Eur Soc Radiology 2011. Oroantral Fistulas. CT Evaluation with Dentascan software
Int J Dent Clinics 2011. Use of Palatal Rotation Flap in the Closure of Oroantral Communication
JUMDC 2012. Case Report. Use of Buccal Fat Pad Oro-Antral Fistula Repair
Open Dent J 2012. Surgical Options In Oroantral Fistula Treatment
JOMS 2013. Treatment of Oro-Antral Fistulas using Bony Press-Fit Technique
J Clin Exp Dent 2015. Alternative Surgical Management of Oroantral Fistula using Auricular Cartilage
Annals of Otolaryngology & Rhinology 2016. Etiology & Management of Oro-Antral Fistula.
J Craniofac Surg 2016. Surgical Treatment of Oro-Antral Communications
Intech 2016. Management of the Oroantral Fistula
World J Plast Surg 2017. Management of Oro-antral Communication & Fistula – Various Surgical Options
Int J Adv Res 2018. Treatment Techniques for Oro-Antral Communications & Fistulas