Local Anæsthetic Allergy & Testing
Following the administration of a local anæsthetic, a minority of patients may suffer one of a range of unwanted symptoms.
Some of these symptoms can be mistaken for hypersensitivity or allergy & the patient unnecessarily told they are allergic to the anæsthetic. Mislabelling of patients as allergic to local anæsthetic can lead to problems for dentists with patients unable to undergo routine dental treatment.
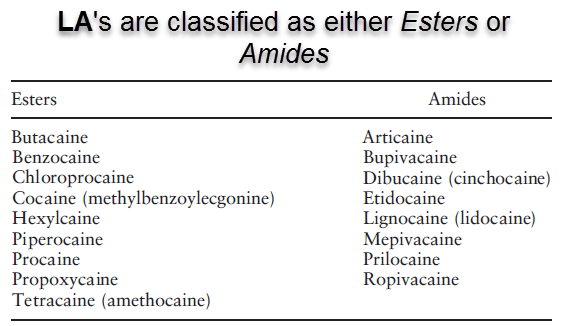
Local Anæsthetics can be categorised into 2 classes:
1. Amides (lidocaine, bupivacaine, prilocaine, ropivacaine, articaine, mepivacaine) &
2. Esters (benzocaine, cocaine, procaine, tetracaine).
True allergy to an amide local anæsthetic is exceedingly rare.
Local anæsthetics of the ester type are more likely to produce allergic reactions as they are metabolised to para-aminobenzoic acid (PABA) which is an allergenic compound. The only ester local anæsthetic used in dentistry is benzocaine, which is used in topical preparations applied prior to administration of local anæsthetic injections.
An allergy to one ester local anæsthetic contra-indicates the use of another ester, as the metabolism of all esters yields PABA.
Patients are unlikely to show cross sensitivity to amide local anæsthetics as these are not metabolised to PABA.
Allergy to one amide local anæsthetic does not contra-indicate use of another amide local anaesthetic. However, it would be unwise to use another amide local anæsthetic without hypersensitivity tests.
Local anæsthetic are considered relatively safe but, given the high number of injections that are administered, adverse reactions are inevitable.
Adverse systemic reactions to local anæsthetics can be divided into 3 categories:
- Allergy
- Psychogenic
- Signs
Symptoms of Local Anæsthetic Hypersensitivity
A true allergy to local anæsthetics may be either type I or type IV.
Type I; immediate anaphylactic reactions mediated by IgE antibodies. Signs and symptoms of Type I Allergy tend to occur within minutes of giving the injection:
- The lips & peri-orbital areas swell (angio-œdema)
- The patient may become agitated & there is generalised urticaria (“hives”) & pruritus (itchiness), particularly of the hands & feet. Other symptoms include abdominal cramps, nausea & diarrhœa
- Tightness of the chest, with wheezing & dyspnœa (difficulty in breathing) may occur
- There may be a fall in blood pressure & a rapid thready pulse, which may be accompanied by flushing of the skin or rash.
Type IV; delayed hypersensitivity reactions mediated by sensitised lymphocytes (“white blood cells”):
- Usually localised to the injection site
- Commonly expressed as a contact dermatitis
Alternative Diagnoses
Genuine hypersensitivity reactions to local anæsthetics are extremely rare.
It has been estimated that true allergic reactions to local anæsthetics account for < 1% of all adverse reactions to local anæsthetics. It is unclear where this figure originates from or the number of patients this represents, as the incidence of adverse reactions occurring in patients who have received local anæsthetics is not reported.
Adverse reactions commonly mistaken for hyper-sensitivity reactions include syncope (fainting), panic attacks & toxic effects due to inadvertent entry of the drug into the circulation.
The following are possible differential diagnoses and their symptoms:
- Allergy
Many allergic reactions involving local anæsthetic preparations are due to other constituents in the injection solution rather than to the drug itself such as preservatives (e.g. benzoates – used in multi-dose vials) & anti-oxidants (e.g. meta-bisulphites, used in local anæsthetic solution containing adrenaline) can cause allergic reactions.
Allergy to latex contained in rubber bungs, natural rubber latex gloves, rubber dams & other dental materials should also be considered.
Historically, the most sensitising components in local anæsthetic solutions were preservatives such as methylparabens. Parabens are no longer added to dental local anæsthetic solutions available in the UK.
- Psychogenic
Psychogenic reactions (originating in the mind, an emotional response) are one of the most common adverse reactions associated with local anæsthetic use in dentistry.
They may manifest in many ways, the most common being syncope but other symptoms include panic attack, hyper-ventilation (rapid breathing), nausea (feeling sick), vomiting & alterations in heart rate or blood pressure, which may cause pallor (paleness).
They can be misdiagnosed as allergic reactions & may also mimic them with signs such as flushing of the skin, blotchy red rash, & œdema (swelling) & broncho-spasm (shortness of breath). All patients have some degree of autonomic response to injections, ranging from slight tachycardia (increased heart rate) & sweating to syncope (fainting).
- Toxic
Toxic reactions may occur if high levels of local anæsthetic enter the blood stream. Local anæsthetics can reach the systemic circulation as a result of repeated injections, inadvertent intra-vascular administration or overdose in those patients who have problems eliminating or metabolising the local anæsthetic.
Toxic side effects are predominantly neurological & include excitability / agitation, sedation, light-headedness, slurred speech, mood alteration, diplopia (double vision), disorientation & muscle twitching. Higher blood levels may result in tremors, respiratory depression & seizures.
Vaso-constrictor agents such as adrenaline may also cause adverse effects. & Adrenaline toxicity can result in symptoms such as anxiety, restlessness, trembling, pounding headache, palpitations, sweating, pallor, weakness, dizziness & respiratory distress.
Toxic reactions can be minimised by staying within safe dosage parameters & using safe injection techniques.
Management Options To Prevent Adverse Effects Occurring
When a patient experiences signs & symptoms that are suggestive of an allergic reaction, possible alternative causes should be considered such as contact with other common allergens, toxic dose or a psychogenic reaction.
The possible causes of the symptoms experienced should be discussed with the patient.
Use of the terms “allergic” & “allergy” should be avoided when discussing any adverse event as these terms are recognised by patients & readily adopted as the explanation.
Adverse reactions caused by toxicity or anxiety can be minimised by:
- Administering injections with an aspirating syringe to avoid intra-vascular injection.
- Relaxing nervous patients to relieve their anxiety. For extremely anxious patients, sedation may be required.
- Treating patients in a supine position to prevent fainting.
- Giving injections slowly to reduce discomfort & improve localisation of solution.
- Restricting the total dose given to the patient to prevent toxic effects occurring by overdose. The maximum dose for the individual patient can be calculated using the dosage information contained in the package insert or recognised dental textbooks on local anæsthetics & taking into account the age & weight of the patient, any concomitant drug therapy & underlying medical conditions.
Management of a Patient Who Suffers an Adverse Reaction in the Surgery
Psychogenic reaction:
- If a fall in blood pressure occurs or the patient feels faint, laying the patient flat & elevating the legs should be sufficient to help restore the blood pressure.
- Any tight clothing around the neck should be loosened.
- Once conscious, the patient should be given a glucose drink.
- Calm the patient and reassure them.
Toxic reaction:
- Symptoms caused by toxicity will be short-lived in most patients. The pharmaco-kinetics of the local anæsthetics used in dentistry suggest that the drug will be eliminated from the blood stream within a couple of hours, but may be as long as 12 hours in some individuals.
- Reassure the patient that they will feel better after several hours & inform them that although the reaction is unpleasant, it should not happen again & it is not necessary to avoid that local anæsthetic in the future.
Management of a Patient When Local Anæsthetic Allergy Is Strongly Suspected
If symptoms suggestive of a true allergic reaction occur (localised reaction consisting of swelling, erythema, an itchy rash or systemic features such as dyspnœa, wheezing, widespread skin rash or circulatory collapse), the patient should be given emergency treatment following the Emergency Treatment Of Anaphylaxis Guidelines [www.resus.org.uk/pages/medental.htm].
If the patient feels unwell, their condition is deteriorating or they are very distressed, they should be transferred to hospital.
The patient should be referred for further investigation to confirm if the local anæsthetic or another possible allergen (e.g. preservative or latex) was the cause of the adverse effects.
If the cause of the symptoms is uncertain, dentists should contact the local (dental) hospital to discuss referring the patient for further investigation.
Alternatively, if a true allergic reaction is suspected, patients can be referred by the dentist or GP directly to the ‘allergy clinic’ at their local hospital, if this service is available.
Location and contact details for allergy clinics can be found via the British Society for Allergy and Clinical Immunology website [www.bsaci.org]. Alternatively, several dental hospitals run this service (such as Guy’s Dental School).
Very rarely, allergy to the local anæsthetic is confirmed. In these cases, immunological testing should be extended to other Local anæsthetics in order to identify a safe alternative for future dental procedures.
Management of Patients who Report to be Allergic to Local Anaesthetic Agents
New patients who claim to have had an allergic reaction to a local anæsthetic should be carefully questioned to obtain a history of past events.
These details may be more reliably obtained from the patient’s previous dentist.
Questions to ask the patient or previous dentist include:
- What symptoms did the patient experience?
- What explanation for the symptoms was given at the time?
- Who told them this?
- Have they ever had any other dental treatment or surgery in the past that required them to have a local anæsthetic? What happened?
- Have they any other allergies?
- Have they ever been tested for a local anæsthetic allergy? If so, what was the result? (The allergy specialist should be contacted for confirmation and further information).
Management:
If further information obtained strongly suggests an allergy but no details are available, refer the patient for allergy testing.
If further information strongly suggests a psychogenic reaction, proceed with care & address the patient’s anxiety.
If further information strongly suggests toxicity, proceed with care starting with low doses of local anæsthetic / vaso-constrictor.
If no information is available from the patient or dentist, contact the GP who may have information about previous local anæsthetic exposure or other relevant knowledge.
If it is strongly suspected that the patient has previously suffered an allergic reaction to a local anæsthetic & emergency dental treatment is required, consider contacting a local hospital Dental / Oral Surgery department to discuss management & referral to a unit that has full resuscitation facilities available.
Useful Websites:
British Society for Allergy and Clinical Immunology
Oral Medicine Department, Guy’s Dental Hospital
Useful Articles:
Anesth Prog 1987. A Guideline to Local Anesthetic Allergy Testing
Anesth Prog 1997. The Incidence of Complications Associated with Local Anesthesia in Dentistry
BDJ 1999. Case Study. Allergic Reactions to Lignocaine
Allergol & Immunopathol 2002. Allergy to Local Anaestheics in Dentistry. Myth or Reality?
Dent Clin N Am 2002. Adverse Drug Reactions to Local Anesthesia
Can J Anaesth 2003. Editorials. Allergies to Local Anaesthetics. The Real Truth
CDAJ 2006. Local Anesthetics – Dentistry’s Most Important Drugs, Clinical Update 2006
Am J Med Sci 2007. Approach to Patients with Suspected Hypersensitivity to Local Anesthetics
Oral Maxillofacial Surg Clin N Am 2013. Management of Allergy & Anaphylaxis During Oral Surgery