Oral Cancer – Referral of Patients with Suspicious Lesions
The Pathway of Care shows how a patient with a (District General Hospital) and seen within 2 weeks (in the UK).
If the lesion is thought to be suspicious, then investigations, imaging ± biopsy are carried out.
The biopsy results are ‘fast-tracked’ and the patient would be seen with the histological results of the biopsy, investigations & imaging results at the MDT (Multi-Disciplinary Team) meeting (held in my area, down at Maidstone Hospital, Kent).

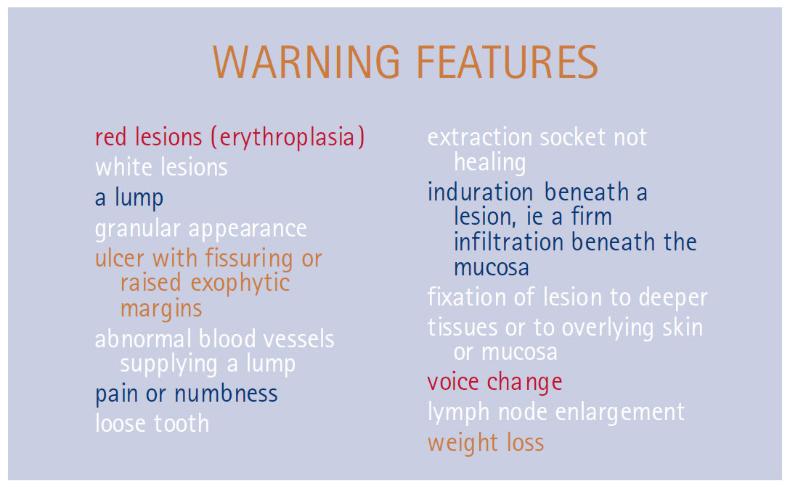
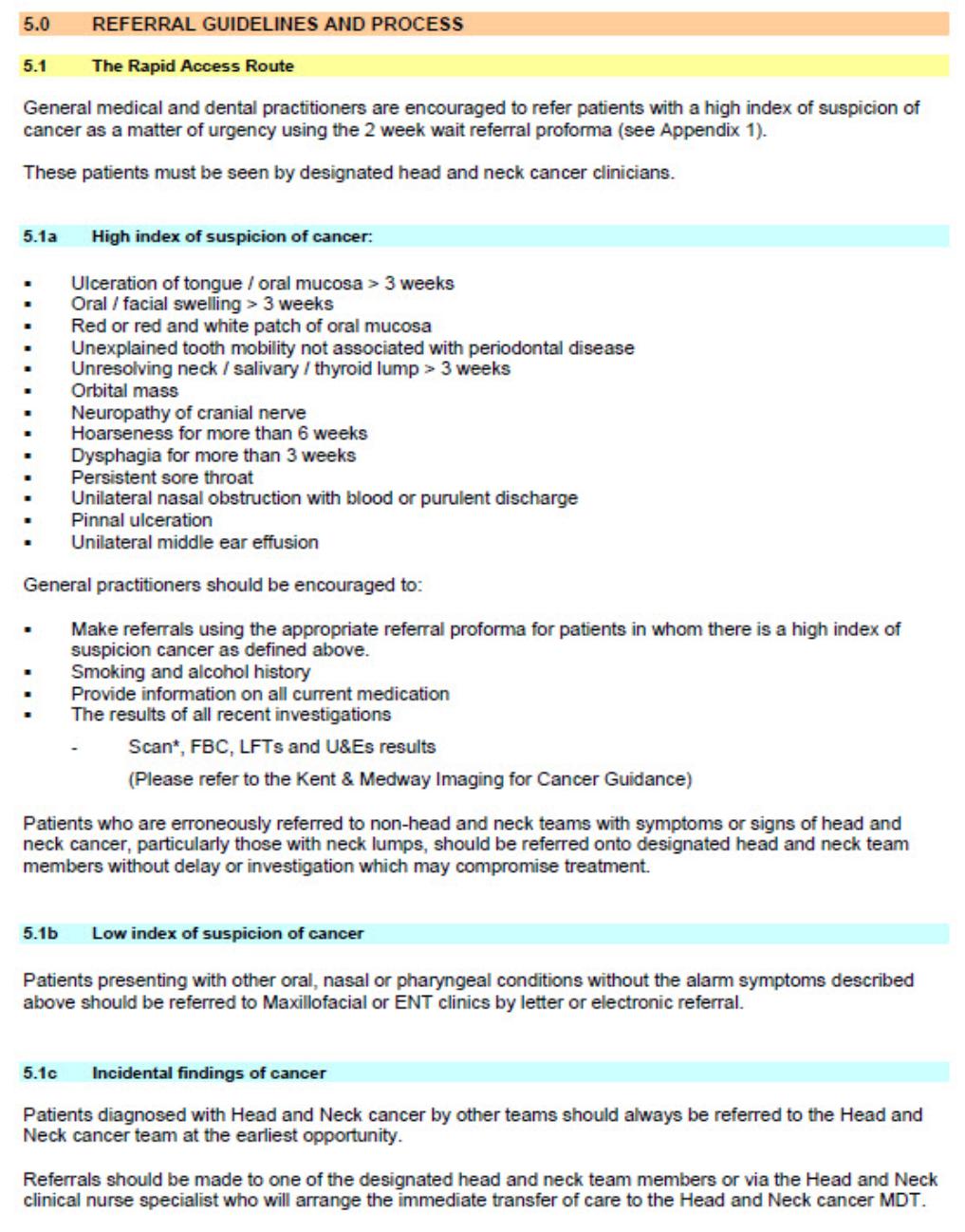
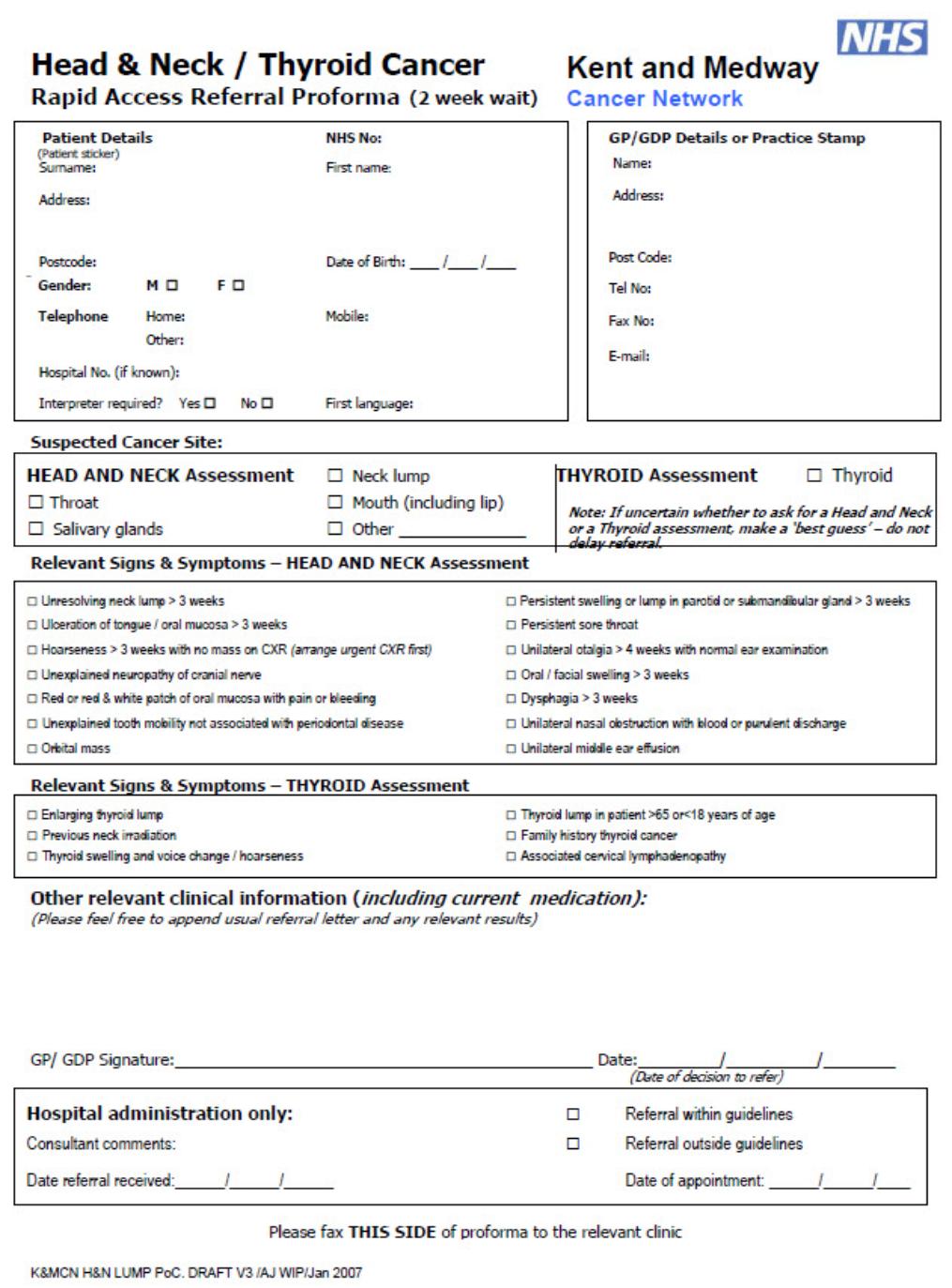
 The suspicious features that the GDP should be aware of are listed here (high-lighted in yellow); these are in a box on the Rapid Referral Form.
The suspicious features that the GDP should be aware of are listed here (high-lighted in yellow); these are in a box on the Rapid Referral Form.
The Pathway of Care shows how a patient with a (District General Hospital) and seen within 2 weeks (in the UK).
If the lesion is thought to be suspicious, then investigations, imaging ± biopsy are carried out.
The biopsy results are ‘fast-tracked’ and the patient would be seen with the histological results of the biopsy, investigations & imaging results at the MDT (Multi-Disciplinary Team) meeting (held in my area, down at Maidstone Hospital, Kent).
The suspicious features that the GDP should be aware of are listed here (high-lighted in yellow); these are in a box on the Rapid Referral Form.
The Pathway of Care shows how a patient with a (District General Hospital) and seen within 2 weeks (in the UK).
If the lesion is thought to be suspicious, then investigations, imaging ± biopsy are carried out.
The biopsy results are ‘fast-tracked’ and the patient would be seen with the histological results of the biopsy, investigations & imaging results at the MDT (Multi-Disciplinary Team) meeting (held in my area, down at Maidstone Hospital, Kent).
The suspicious features that the GDP should be aware of are listed here (high-lighted in yellow); these are in a box on the Rapid Referral Form.These are the referral forms for suspected neoplastic / mitotic lesions – these are filled out & sent electronically
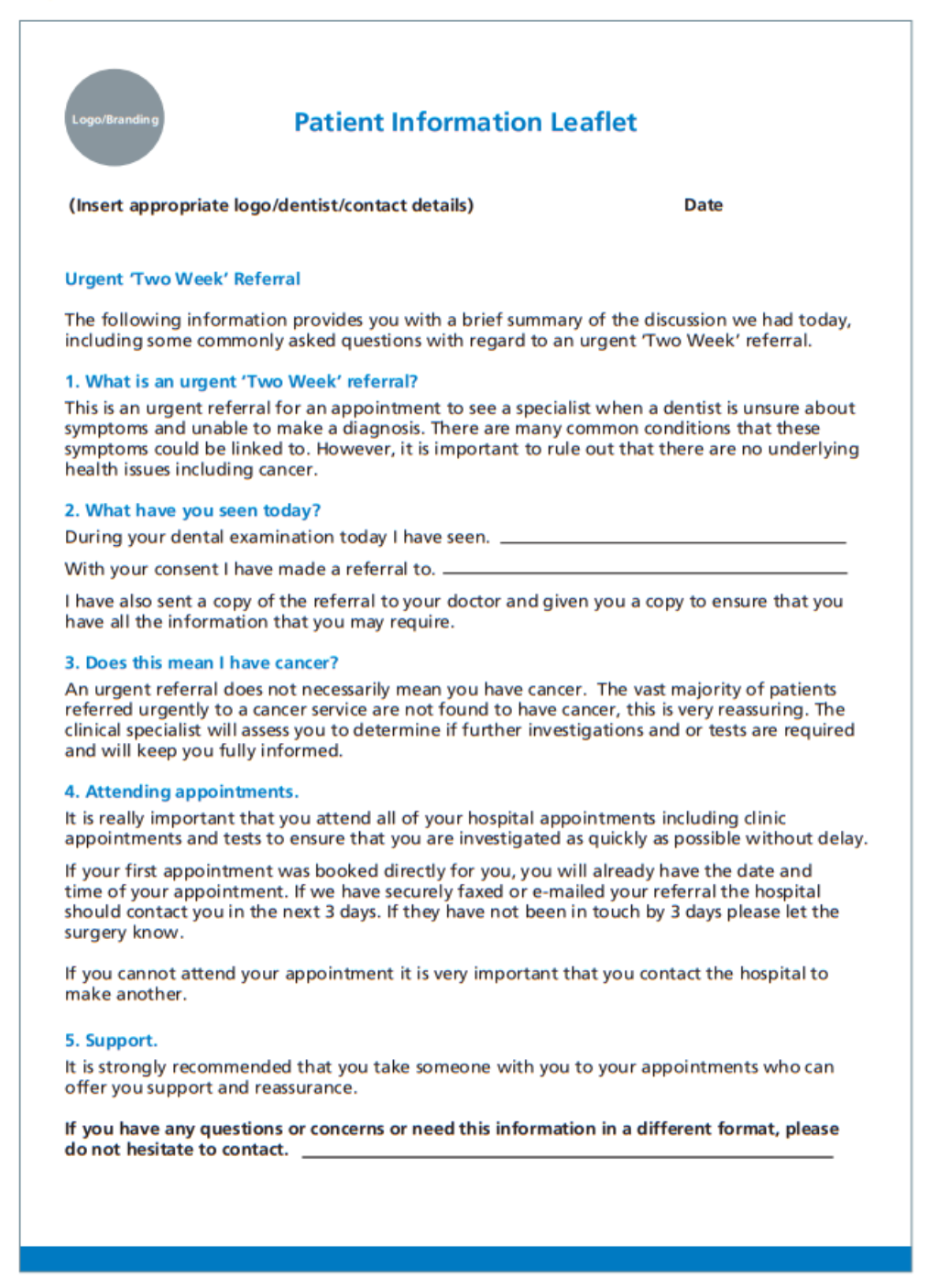
When consulting with your patient it is important that you record clinical status, signs, symptoms, referral process & what information & advice you gave the patient both verbally & in writing.
Records should be kept In-line with authoritative and professional guidance.
 A “best practice” Head & Neck referral
A “best practice” Head & Neck referral
 Information given to a patient should cover:
Information given to a patient should cover:
- What an urgent ‘Two Week’ referral is
- Why the patient is being referred to a 2nd care cancer service
- The percentage of urgent ‘Two Week’ referrals that are cancerous
- Which 2nd care cancer service the patient is being referred to
- How they will receive their appointment
- The importance of attendance
- Whether the patient can take someone with them
- What type of tests / investigations that might be carried out & how long it will take to get results & a diagnosis
- How to obtain further help & information about the type of oral cancer suspected
Useful Articles & Websites
National Institute of Clinical Excellence
J Can Dent Assoc 2008. Biopsy & Histopathologic Diagnosis of Oral Premalignant & Malignant Lesions
Head & Neck Cancer Guidelines 2011
BDJ 2015. Why Don’t Dentists Talk To Patients About Oral Cancer?
Dent Update 2016. Mouth Cancer for Clinicians Part 8. Referral
NICE Guidelines 2017. Head & Neck Cancer
BDJ 2018. Mouth Cancer – Presentation, Detection & Referral in Primary Dental Care
Dental Update 2020. Mouth Cancer – the Maxillofacial Surgeon’s perspective