Cavernous Sinus Thrombosis
Cavernous Sinus Thrombosis (CST) is a rare, life-threatening disorder that can result from facial infections, sinusitis, orbital cellulitis, pharyngitis or otitis or following traumatic injury / surgery, especially in the setting of a thrombophilic disorder.
Early recognition of CST which, often presents with fever, headache, eye findings such as peri orbital swelling & ophthalmoplegia, is critical for a good outcome.
Despite modern treatment with antibiotics & anti-coagulation, the risk of long-term sequelae, such as vision, diplopia & stroke, remains significant.
Causes:
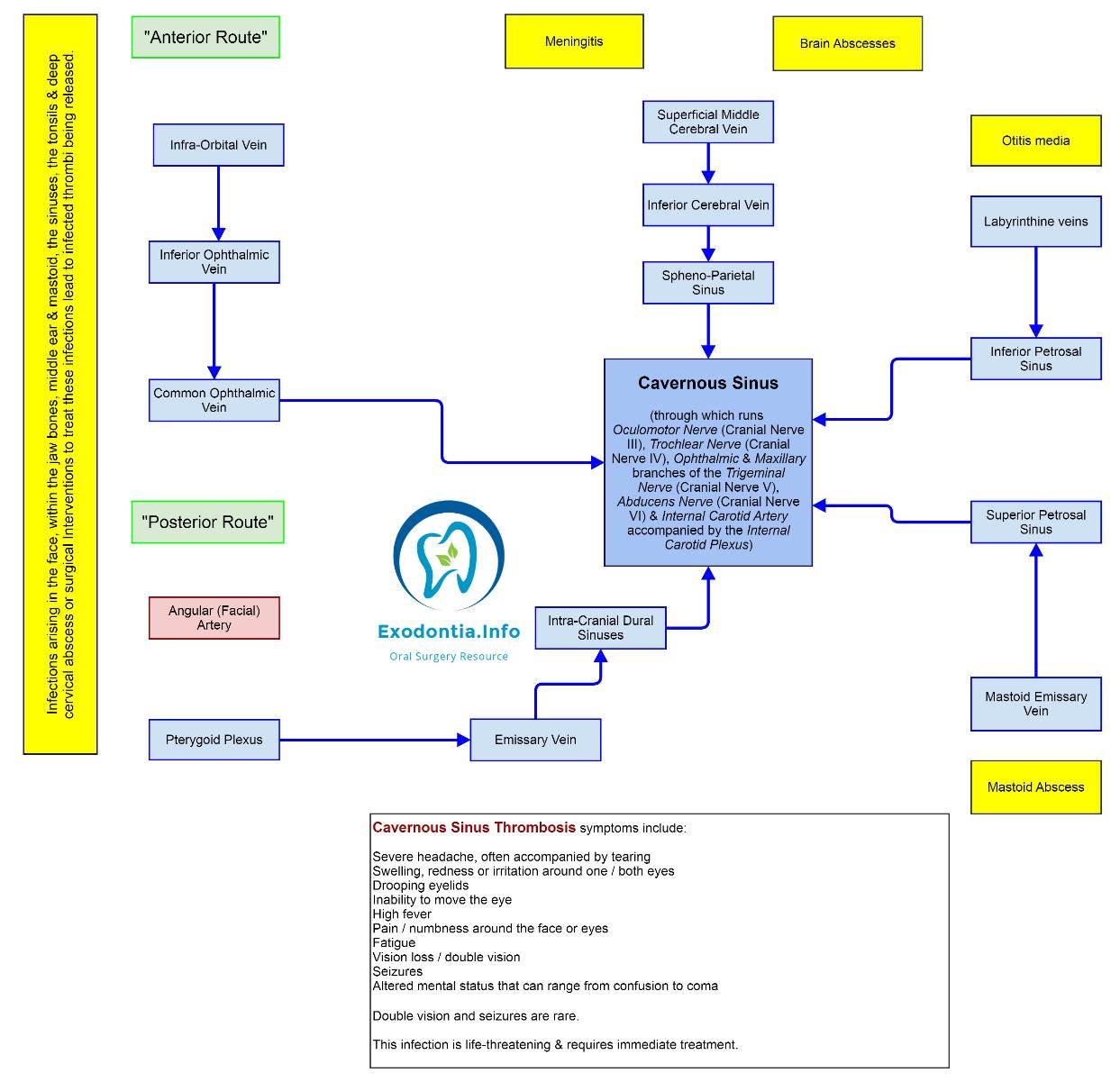
CST is usually septic, but can also be aseptic. Septic cases can follow central facial infections, especially within the “danger triangle” of the face (from the corners of the mouth to the bridge of the nose). These include abscess or cellulitis, sinusitis (especially sphenoiditis and ethmoiditis), dental infections, extractions or procedures (even a posterior superior alveolar nerve block entering the pterygoid plexus), maxillofacial surgery, otitis media & mastoiditis.
Aseptic causes are less common than septic causes. These include trauma, surgery or pregnancy.
A variety of infectious organisms can cause CST although the majority are bacterial. Fungal infection in CST is less common. Rarer still are parasites (such as toxoplasmosis, malaria & trichinosis) as well as viruses (such as herpes simplex, cytomegalovirus, measles, hepatitis & HIV).
Immunosuppression, such as uncontrolled diabetes, steroid use, cancer or chemotherapy, maybe a risk for not only developing CST but also developing complications.
The biggest risk factors are facial infections, acute sinusitis & peri-orbital infections. Thrombophilia is a significant risk factor for CST.
How CST Happens:
The mechanism is due to:
- Embolisation of bacteria & other infectious organisms which trigger thrombosis which then can trap infection within the Cavernous Sinus.
- CST leads to decreased drainage from the Facial Vein & Superior & Inferior Ophthalmic Veins resulting in facial & peri-orbital œdema, ptosis, proptosis, chemosis, discomfort & pain with eye muscle movement, papillœdema, retinal venous distention & loss of vision. Lack of valves in the dural sinus system allows flow through the emissary veins into & out of the Cavernous Sinus & thrombus can propagate into the dural system. Also, communication between the right & left cavernous sinuses via the inter-cavernous sinuses, anterior & posterior to the sella, allows the spread of thrombus & infection from one side to the other.
Local compression & inflammation of cranial nerves can lead to several partial / complete cranial neuropathies including:
- Diplopia from partial / complete external ophthalmoplegia due to compression of the VI (Abducens), III (Oculomotor) and IV (Trochlear) cranial nerves. Limited eye abduction from Abducens palsy is most common early finding, often progressing to inability to move the eye in any direction when III, IV and VI cranial nerves are involved
- Internal ophthalmoplegia (non-reactive pupil) occurs from loss of sympathetic fibres from the short ciliary nerves (resulting in miosis) and / or from loss of para-sympathetic fibres from cranial nerve III (resulting in mydriasis)
- Anæsthesia / paræsthesiæ (around the eyes, nose, forehead) & loss of corneal blink reflex from the Ophthalmic Nerve, a branch of the Trigeminal Nerve (V)
- Facial pain, paræsthesiæ / anæsthesia from compression of the maxillary branch of the Trigeminal Nerve.
- Septic Cavernous Venous Thrombosis can result in the central nervous system or infectious pulmonary complications.
Because the dural venous & cavernous system is valveless, this venous blood can communicate with the dural sinuses & cerebral & emissary veins leading to meningitis, dural empyema or brain abscess.
Infection can spread via the jugular vein to the pulmonary vasculature resulting in septic emboli or abscess, pneumonia or empyema.
Stroke can occur following carotid artery narrowing, vasculitis, or haemorrhagic infarction following progression to cortical vein thrombosis.
Hypo-pituitarism can occur due to ischaemia or the direct spread of infection.
Useful Articles & Websites
JRMS 2010. Cavernous Sinus Thrombosis as a Fatal Complication of a Dental Abscess – A Case Report
BJOMS 2011. Short Communication. Septic thrombosis of the cavernous sinus & dental infection
JOMS 2013. Cavernous Sinus Thrombosis as a Result of a Fungal Infection. A Case Report
Int J Clin Exp Med 2016. Cavernous Sinus Thrombosis of Odontogenic Origin