Release of Salivary Stones
What are (Submandibular / Sub-lingual) Salivary Gland Stones?
Sialolithiasis (Salivary Gland Stones) is the most common disease of the salivary glands. It is affects 12 in 1000 of the adult population; men are affected twice as much as women; children are rarely affected.
Sialolithiasis accounts for more than 50% of diseases of the large salivary glands and is thus the most common cause of acute and chronic salivary gland infections. More than 80% occur in the Submandibular Gland or its duct, 6% in the Parotid Gland and 2% in the Sublingual Gland [link to Sublingual Gland Removal webpage] or minor salivary glands.
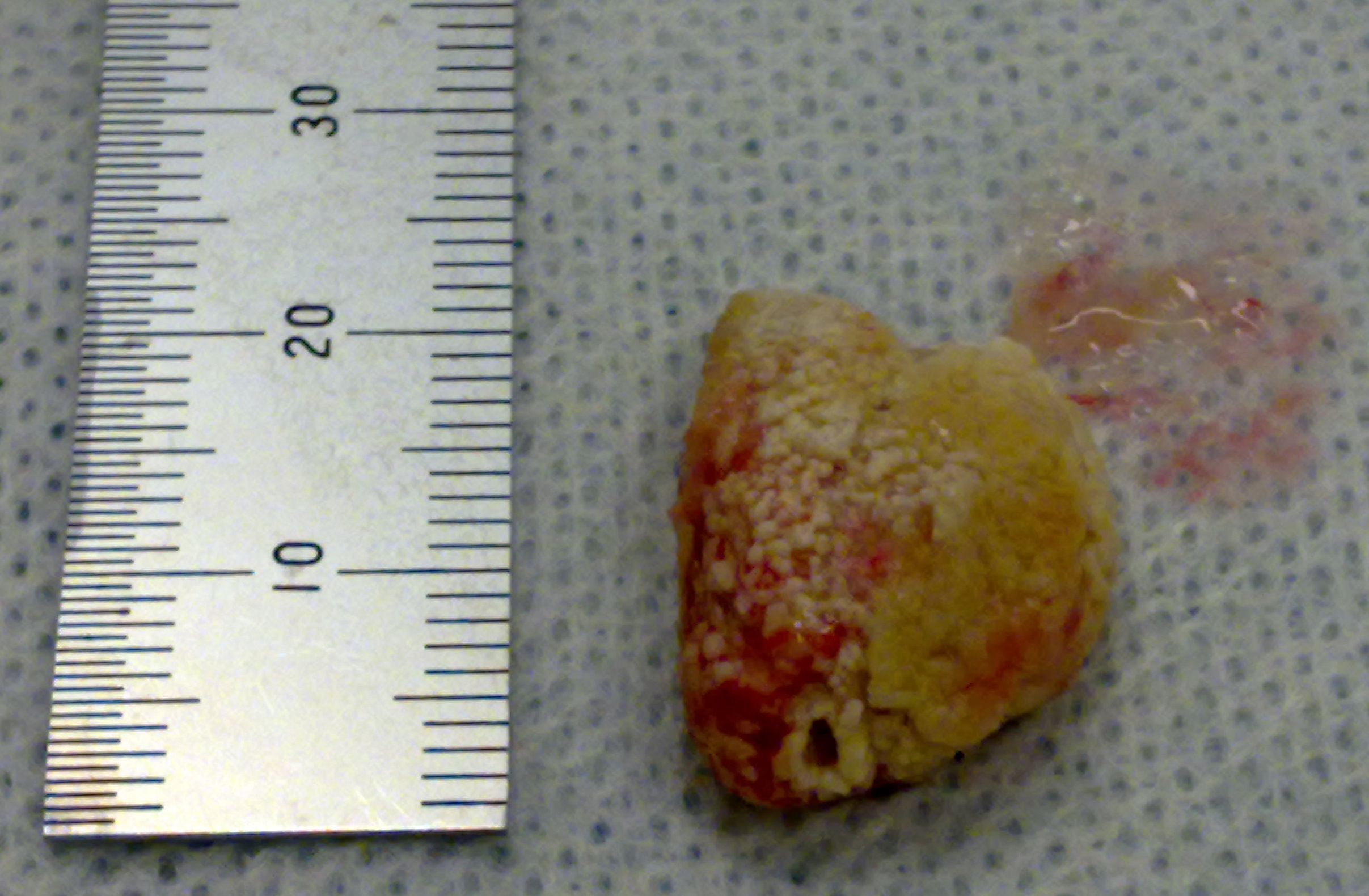
 Photos of Sialoliths removed from the Submandibular Duct
Photos of Sialoliths removed from the Submandibular Duct
Clinical Examination, Investigations & Diagnosis
Careful history and examination are important in the diagnosis of sialolithiasis (in fact, in all aspects of medicine & dentistry). Pain and swelling of the concerned gland at meal-times and in response to other salivary stimuli are especially important. Complete obstruction of the salivary duct by a salivary stone causes constant pain and swelling; pus may be seen draining from the duct and signs of systemic infection may be present.
Bi-manual palpation of the floor of the mouth, in a posterior (back) to anterior (front) direction, reveals a salivary stone in a large number of cases of Submandibular Calculi Formation. Bi-manual palpation of the gland itself can be useful, as a uniformly firm and hard gland suggests a hypo-functional (under-performing) or non-functional gland.
Imaging studies are very useful for diagnosing sialolithiasis. Occlusal radiographs (X-rays of the floor of the mouth) are useful in showing (radio-opaque) stones.
Sialography is useful in patients showing signs of sialadenitis related to (radio-lucent) stones or deep submandibular / parotid stones. Sialography is, however, contra-indicated in acute infection or in marked contrast allergy (i.e. an allergy to the contrast media pumped into the duct and gland).

What does the treatment involve?
There are various methods available for the management of salivary stones, depending on the gland affected and stone location.
Patients presenting with sialolithiasis may benefit from a trial of conservative management especially if the stone is small.
The patient must be well hydrated (that is, drink frequently) and must apply moist warm heat and massage the involved salivary gland, while sialogogues are used to promote saliva production and flush the stone out of the duct.
With gland swelling and sialolithiasis, infection should be assumed and antibiotics prescribed. Most stones will respond to such a regimen, combined with simple sialolithotomy when required.
If the stone is sufficiently forward in the salivary duct, it can be “milked” and manipulated through the duct opening; this can be done with the aid of lacrimal probes and dilators to open the duct.
Once open, the stone can be identified, “milked” forward, grasped and removed. The gland is then “milked” to remove any other debris in the more posterior (back) portion of the duct.
Almost half of the Submandibular Calculi lie in the distal third of the duct and are amenable to simple surgical release through an incision (cut) directly onto the stone. In this way more posterior stones, 1 – 2 cm from the salivary duct punctum, can be removed by cutting directly onto the stone in the longitudinal axis of the duct. Care is taken as the Lingual Nerve. lies deep to the duct, but in close association with the Submandibular Duct posteriorly. Subsequently, the stone can be grasped and removed. No closure is done leaving the duct open for drainage.
If the Submandibular Gland has been damaged by recurrent infection and fibrosis or calculi have formed within the gland, the gland may require removal.
Alternative methods of treatment have emerged such as the use of Extracorporeal Shock Wave Lithotripsy (ESWL) and more recently the use of Endoscopic Intracorporeal Shockwave Lithotripsy (EISWL), in which shockwaves are delivered directly to the surface of the stone lodged within the duct without damaging adjacent tissue (piezoelectric principle). Both extra and intra-corporeal lithotripsy are gaining increasing importance in the treatment of Salivary Stone Disease.
Submandibular Gland Removal may be indicated following failure of lithotripsy or if the size of an intra-glandular stone is > 12 mm as the success of lithotripsy may be < 20% in such cases.
In the case of small calculi, the treatment of choice should be medical, instead of surgical. The patient can be administered natural sialogogues such as small slices of lemon or sialogogue medication (such as pilocarpine) removal.
Surgical removal of the calculus (or even of the whole gland) has traditionally been used as an alternative to medical therapy, whenever the latter was not possible or when it proved ineffective.
How long will the operation take?
It can be very quick (a few minutes). If the stone is big or difficult to access, it can take that much longer.
What can I expect after the operation?
It is unlikely to be very sore but regular painkillers will be arranged for you. There is relatively little swelling following salivary stone removal.
Do I need any time off work?
Possibly only for the day of the operation.
Will I have a scar?
No.
What are the possible complications?
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
There are potential complications with any operation. Fortunately, with this type of surgery complications are rare and may not happen to you.
The following list of warnings regarding sialolith release is neither exhaustive nor is it predictive. The most pertinent warnings have been included here.
- Pain [link to Postop Analgesia webpage]. As it is a surgical procedure, there will be soreness at the operation site. This can last for several days. Painkillers such as Ibuprofen, Paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history and the ease with which the stone was released.
- Swelling. There will be swelling afterwards though it will not be obvious from the outside. Sucking an ice-cube at the op site will help to decrease the swelling. Avoidance in the first few hours post-op of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that can develop.
- Sutures. The op site will often be closed with stitches. These dissolve and “fall out”; within 10 – 14 days.
- Limitation of Mouth Opening . Often the chewing muscles and the jaw joints are sore after the op so that mouth opening can be limited for the next few days.
- Scarring / Lumpiness at Op Site. Any cut to soft tissues produces a scar. Initially, after the release of a stone, a scar may be produced. This softens and disappears (i.e. improves) with time. The scarring can also be dependent on the size of the stone, how long it had been present for, how many infections had been associated with it and the individual’s tendency to scarring.
- Floor of Mouth Complications. When stitching up the operation site, sometimes, the stitches can tie off the Submandibular Duct. If this happens, saliva produced by the Submandibular Gland cannot escape into the mouth and back pressure into the gland happens. This causes the Submandibular Gland to swell and become painful. The floor of the mouth may even rise.
- If any of this happens, you will need to contact the OMFS department or A&E as soon as possible. Because of the potential of this to happen, stitches are sometimes not used or if used, are very loose.
- Repeat Op. Sometimes not all of the stone is removed or there were more stones than originally thought (and not obvious on the X-ray) or the conditions that created the salivary stone in the first place haven’t changed and a new stone has formed; hence, the need to repeat the op.
- Numbness of the Tongue. The Lingual Nerve which supplies feeling to the side of the tongue can become bruised as a result of surgery. If this occurs you will experience a tingly or numb feeling in the tongue, similar to the sensation after having an injection at the dentist. This numbness may take several months to disappear and in a minority of patients may last for ever.
- Damage to the Submandibular Duct. The Submandibular Duct is the name of the tube which carries saliva from the Submandibular Gland into the mouth. The duct runs close to the Sublingual Gland before opening on the inside of the mouth under the tongue immediately behind the lower front teeth. If this duct is damaged, saliva may not drain properly from the Submandibular Gland and the gland may therefore swell in the upper part of the neck. The majority of these swellings settle down on their own.
- Need for Gland Excision. If the stone has caused multiple infections in the Submandibular Gland, this may have damaged the gland so much that removal of the stone will have no beneficial effects. If this is the case, the Submandibular Gland may need to be removed.
Are there are any long-term effects of having my (Submandibular / Sub-Lingual) salivary stones removed?
No.
Will I need further appointments?
Not necessarily. If the stone has been removed and it is thought that all the stone has been removed and that the procedure was straightforward, then there is no need for review. If there are any queries, then a review is most likely.
Useful Articles & Websites
European Association of Oral Medicine
Turk J Med Sci 2001. Sialolithiasis (Salivary Stone)
British Dental Journal 2002. Sialolithiasis. An unusually large submandibular salivary stone.
Arch Otolaryngol Head Neck Surg 2003. Sialolithiasis Management – The State of the Art.
Eastman Dental Institute Oral Medicine Clinic (2004). Obstructive Salivary Disease.
JOMS 2004. Submandibular Salivary Stones – Current Management Modalities
Acta Otorhinolaryngol Ital 2005. Current Opinions In Sialolithiasis – diagnosis and treatment.
Dental Update 2006. A Revolution in the Management of Obstructive Salivary Gland Disease.
JOMS 2007. Giant Sialolith – Case Report and Review of the Literature
Acta Oto Rhinolaryngologica Italica 2007. Review. Modern management of obstructive salivary diseases
Patient UK (2008). Salivary Gland Stones (Salivary Calculi)
ENTNews 2008. Salivary Gland Obstruction, Changing Patterns of Practice.
BJOMS 2008. Selective management of obstructive submandibular sialadenitis
BJOMS 2009. Recent advances in the management of salivary gland disease.
Otolaryngol Clin N Am 42 2009. Alternatives for the Treatment of Salivary Duct Obstruction
J Oral Maxillofac Surg 2010. Modern Sialography for Screening of Salivary Gland Obstruction.
NEJM 2011. Images in Clinical Medicine. Sialolith of the Submandibular Salivary Gland
BDJ 2014. Salivary Stones – Symptoms, Ætiology, Biochemical Composition & Treatment
JOMS 2014. Interventional Sialoendoscopy for Treatment of Obstructive Sialadenitis
BDJ 2015. Oral Surgery. Self-Milking the Sialolith
J Contemp Med Sci 2018. Gold Standard Approach for Removing Sialoliths from the Submandibular Gland
Intl Dent J Student Res 2019. Anterior Submandibular Sialolithiasis. A Series of 5 Cases
Dent Update 2020. A Sialolith and a Megalith – A Report of 2 Cases